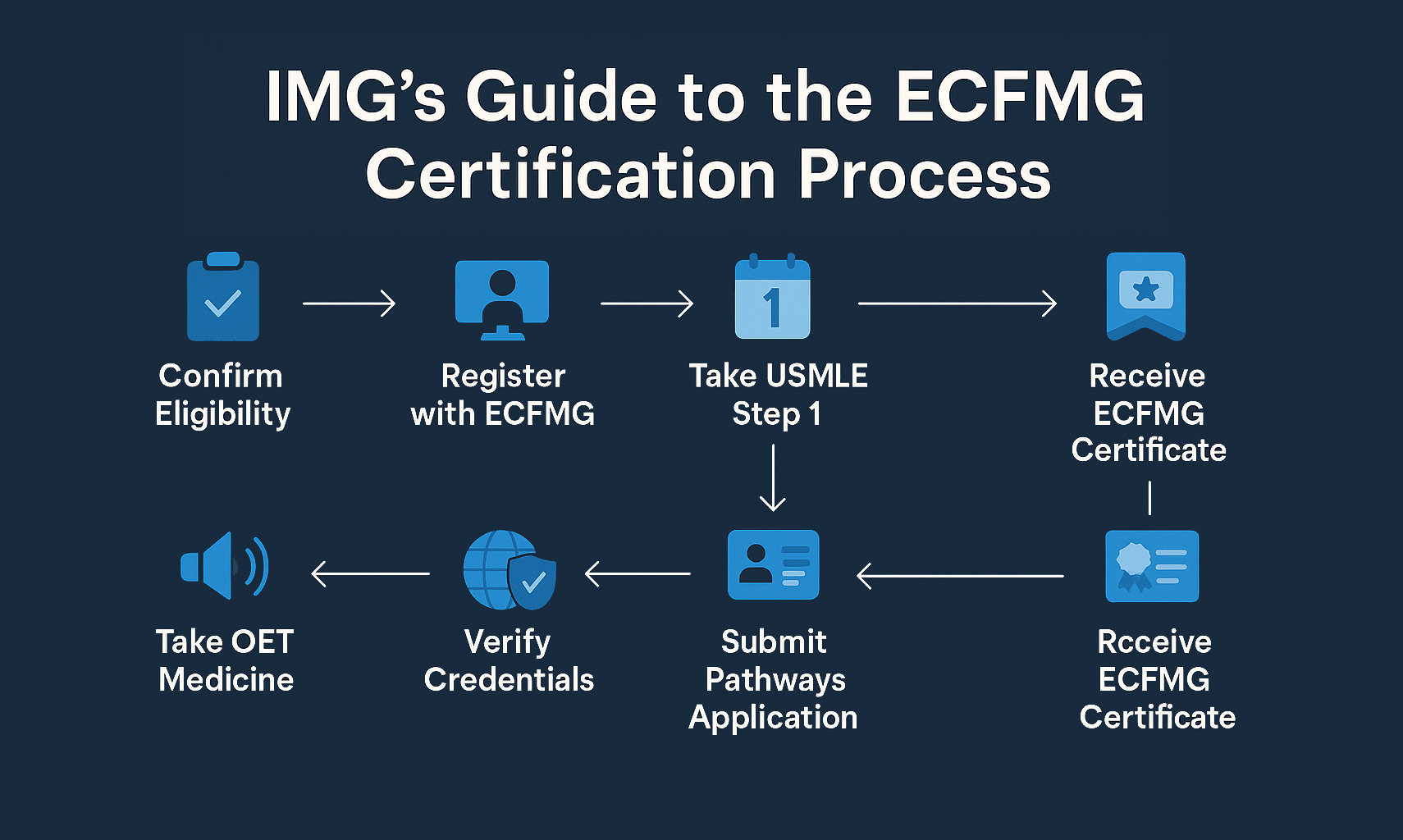
Goal: align your ECFMG certification, USMLE testing, and document logistics with the ERAS/NRMP calendar so eligibility never blocks an interview or rank. Work backward from when programs open applications (late September) rather than from Match Week. For most IMGs, a realistic run-up is 9–12 months. Month −12 to −9: Confirm eligibility. If you are not yet ECFMG certified, map your certification Pathway (1–6) and the communication-skills requirement (OET Medicine). Book OET early (results turn around quickly, but retakes compress calendars). In parallel, set a Step 2 CK target date that leaves ≥8 weeks for score release before application submission. Establish an EPIC/primary-source verification plan for credentials and designate ECFMG to transmit your USMLE transcript to ERAS. Begin collecting proof documents you will need (diploma/expected graduation letter, passport ID page, name-change documents if applicable). Month −9 to −6: Secure USCE. Prioritize hands-on electives or sub-internships when possible; otherwise, organized observerships with defined roles and measurable outputs (mini-QI, case logs). Identify two letter writers from USCE and one from home institution or research; brief them on your specialty narrative and deliver a bulletized accomplishments sheet. Draft personal statement v1; start a journal of cases/behaviors for interview stories. Month −6 to −3: Sit for Step 2 CK; if feasible, schedule Step 3 for visa-friendly fields (some H-1B programs prefer completion). Create your program list scaffold from three tiers (aspirational/core/safety); track historical visa sponsorship and IMG match rates. Prepare program-specific blurb banks (75–100 words) for ERAS experiences and signals. Book OET (or retake) if outstanding. Polish CV bullets: outcomes → scale → role → tools. Month −3 to −1: Lock in ECFMG Pathway documentation, submit OET scores, and monitor OASIS for status changes. Finalize ERAS: proof every section, upload PS and letters, and pre-assign documents. Draft signal allocations by specialty rules; pre-write interview day questions and a rank-notes template. Confirm time-zone readiness for virtual invites and ensure your voicemail/email are professional. Submission month: Submit early in the opening window; avoid last-minute uploads. Track interview invites with a simple CRM (sheet with columns for date, action, follow-up). When you receive an interview, immediately block travel/time zones and send a concise confirmation with any needed accommodations (religious observance, caregiving, disability) per program instructions. Step profile realities. Step 1 is now pass/fail; committees lean harder on Step 2 CK (and occasionally Step 3) to benchmark readiness. Interpret your Step 2 CK in context: percentile bands matter more than raw numbers across specialties. Use recent specialty charts (program fill rates, IMG composition, signal impact) to estimate interview probability by tier. If you have an attempt or a gap, anchor your narrative to remediation and trajectory: what changed in your study design, what metrics improved, and how that maps to the PGY-1 environment. Signal economics. Preference signaling is a scarce resource; think of each signal as a targeted experiment to convert in the interview funnel. First, define your “core fit” predictors: visa sponsorship history, IMG alumni, size of program, and geography where you have social support. Second, pre-match your signals to these predictors; third, prepare 75–100-word notes that link your experiences to that program’s patient population, research, or curricular features. Avoid spraying signals at purely “brand-name” programs unless your dossier already aligns (home research, faculty contacts, geographic ties). How many programs? Balance breadth with depth. Over-applying dilutes your capacity to customize documents and exhausts letter writers; under-applying risks interview scarcity. The right number depends on specialty competitiveness and your profile. As an IMG, consider building a three-ring list: 20–30 core programs with clear fit and visa support; 10–15 aspirational programs where distinct assets make you compelling (research niche, language skills); and 10–15 safety programs aligned to your strengths and location flexibility. For ultra-competitive fields, expand each ring by ~25% and emphasize research continuity and sub-specialty alignment. Score-informed pivots. If Step 2 CK returns below target for your primary specialty, you have options: 1) tighten geographic focus and strengthen USCE/letters in those programs; 2) complete Step 3 to signal readiness where it is valued (particularly H-1B-friendly programs); 3) consider an adjacent specialty that leverages your assets (e.g., strong chronic-disease management and multilingual communication → Family Medicine; procedural enthusiasm with solid anatomy scores → General Surgery prelim, with a categorical re-entry plan). Whatever you choose, keep your story consistent: mission, population, and training environment. USCE is signal, not just seat time. Programs read USCE as evidence you understand U.S. workflows (EHRs, handoffs, pages, consult etiquette) and can contribute without heavy onboarding. Convert even short observerships into measurable outcomes by negotiating a micro-project: e.g., updating an order set under supervision, building a patient-education handout, or auditing time-to-antibiotics for febrile neutropenia with a simple run chart. Log the data, then craft a brief impact statement that a letter writer can cite. Engineering strong letters. Ask early and make it easy to write a detailed letter: provide a one-page “LOR kit” with your CV, personal statement bullet points, your top 3 cases/encounters with your role and results, and a draft paragraph showcasing ACGME competencies (patient care, medical knowledge, systems-based practice, practice-based learning, professionalism, communication). Letters are most credible when they include specific comparisons (“top 10% of rotators in five years”) and time-bound observations (e.g., “over a 4-week inpatient rotation”). Align USCE to specialty narratives. Map each USCE activity to the program’s needs. For IM: volume triage/readiness to manage common admissions; for EM: teamwork and closed-loop communication under time pressure; for Pathology: specimen handling and analytic rigor; for Psych: de-escalation and risk assessment. Translate each into one or two ERAS bullets with outcome → scale → tools → role structure (e.g., “Reduced discharge prescription errors 28% after implementing a two-point ID check; co-designed laminated nursing prompt card”). Red-flag repair. If you have gaps (late graduation, attempts, leave), create an observable improvement arc. Examples: demonstrate sober test-retooling (NBME baseline → spaced repetition → UWorld % → NBME improvement); show sustained performance in USCE (on-time notes, positive patient comments, punctual sign-outs). Prompt letter writers to document these behaviors explicitly—it reframes risk for the committee from “unknown” to “improving under supervision.” Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data. Think like a screener. PDs skim quickly for “can do the work” and “fits our setting.” Structure every experience entry to answer: What changed because you were there? Use compact bullets (max ~20 words) with numerators/denominators, action verbs, and setting. Front-load outcomes and nouns; bury adjectives. Avoid generic claims (“strong teamwork”). Instead: “Co-led rapid-cycle PDSA to cut left-without-being-seen from 8.2%→5.1% over 6 weeks; created handoff script adopted by 3 pods.” Personal Statement (PS). Your PS should be a router, not a memoir. One page, three moves: Anchor (why this field in this system), Evidence (2–3 scenes proving the behaviors programs want), and Bridge (how their curriculum/setting accelerates your goals). End with “how I will contribute on day one,” not future fellowship plans. If visa status is relevant, you can briefly and neutrally acknowledge openness to sponsored pathways without negotiating in prose (“I am authorized to train and open to J-1/H-1B sponsorship per program policy”). Filtering realities. Some programs still apply score/date/visa filters in PDWS. Counter this by ensuring date recency (graduation within 5–7 years if possible), clear visa line in the application, and cohesive letters that reference the same strengths the PS and experiences highlight. Where allowed, upload abstracts/preprints with DOIs; avoid long lists of non-peer-reviewed work unless it shows sustained collaboration or tangible quality improvement. Document order & keywords. Place your most relevant letter first (e.g., inpatient attending for IM, OR attending for Surgery). In the experiences, include keywords committees search for (Epic/Cerner, Epic SmartPhrases, SBAR, handoff, cross-cover, audit/feedback, PDSA, QI, interpreter services, safety huddles). These aren’t buzzwords—they signal readiness for systems-based practice. Know the rules for your specialty. The number and type of signals vary (some use “gold/silver” tiers; others a single pool). Confirm the current cycle’s counts and participating specialties, then lock your plan before submission. Signals work best where your dossier already shows fit—use them to lift your application from “maybe” to “interview.” Three-tier program list. Start with ~40–60 programs (adjust for competitiveness). Assign each program to: Aspirational (brand or stretch metrics), Core (strong mission/geographic/visa fit), or Safety (robust IMG history, broad visa support). Allocate premium (“gold”) signals to the top 10–15 programs in Core where your stories and letters strongly match the case mix or curriculum; distribute remaining signals to a mix of Core and select Aspirational options with faculty or research ties. Keep 2–3 signals unassigned until the final week in case new intel emerges (participation lists update; some programs opt in/out late). Write signal blurbs like mini-cover letters. One specific clinical or curricular hook, one sentence tying your prior work to their population, and one “how I’ll contribute on day one.” Example: “Your safety-net ICU rotation aligns with my QI project cutting CLABSI 23% over 3 months; I’d bring that audit/feedback skillset to your intern X+Y blocks.” Track conversions. Maintain a sheet with columns for program, signal (Y/N; gold/silver), tailored PS (Y/N), alumni contact (Y/N), date sent, response/II status. After two weeks, re-assess: if your interview yield lags, expand the safety ring and increase USCE/professor outreach, not mass emails to PDs. Frameworks that travel across accents and time zones. Use STARR (Situation–Task–Action–Result–Reflection) to keep answers compact and concrete. Cap stories at ~90 seconds; reserve 15 seconds for what you learned and how it generalizes to internship. Build a 10-story “bank” mapped to ACGME competencies (e.g., managing a crashing patient → patient care + communication; near-miss med error → systems-based practice + professionalism). Rehearse on video to optimize pacing and diction; avoid reading from notes. Address common IMG worries up front. Prepare crisp answers for: U.S. clinical workflow (“I’ve written daily notes in Epic during sub-I, responded to pages via Voalte, and practiced SBAR during cross-cover drills.”), communication (“I use interpreter services and teach-back for limited English proficiency; here’s a vignette.”), and visa (neutral, factual, policy-aware: “I am eligible for J-1 and open to H-1B where offered; I will follow your institution’s process.”). Don’t ask programs to make immigration predictions; focus on your readiness to start on July 1 and the steps you control. Virtual logistics. Triple-check time zones. Hard-wire Ethernet if possible, raise your camera to eye level, and place a soft light at 45°. Use a neutral background and silence all alerts. Practice slight over-enunciation and strategic pauses if latency is present; confirm you’re not recording (many institutions prohibit it). Keep water and a notepad nearby; write the interviewer’s name and one program fact as soon as you join. Red-flag, gracefully. If asked about attempts/interruptions, own it, then pivot to concrete repair: “I failed Step 1 in 2021. I audited my process (no spaced review, weak error log), adopted Anki + an error diary, and improved NBME forms by 9–12 points, passing Step 2 CK on the first attempt. Those same habits—daily error reviews, checklists—are how I’ll protect patients on nights.” Concision + trajectory > long justifications. Right after each interview: Within an hour, write structured notes: people (names/roles), clinical strengths (case mix, ICU exposure), educational structure (X+Y, simulation), support (mentorship, IMG alumni), and any concerns (moonlighting, call frequency). Give each program a 1–5 score on training fit, geographic/visa feasibility, and wellness. Draft—but don’t send—thank-you notes unless a program explicitly welcomes them; avoid language that implies a ranking commitment. Post-interview communication. Many programs and applicants misstep here. It’s acceptable to exchange clarifying information (e.g., rotations, benefits, start-date logistics) and to express continued interest if invited, but avoid promising rank positions or requesting the program’s rank intentions. Keep messages brief, professional, and compliant with Match guidelines. If you’re uncertain whether a message is appropriate, default to silence or ask the program coordinator. Rank strategy. Rank in your true order of preference, full stop. Don’t try to “game” perceived interest; the algorithm rewards honest lists. Integrate a risk-balanced approach: ensure your top 10 include multiple programs with IMG alumni and clear visa support. For couples, rehearse multiple joint lists early and identify at least two geographic clusters where both partners would be satisfied. For prelim→categorical bridges, confirm historical success rates and mentorship structures before ranking highly. SOAP contingency. Build a pre-packaged dossier: a 3-paragraph rapid PS per specialty pivot, an updated CV, transcript permissions, and a 1-page “strengths snapshot” (metrics, USCE highlights, visa status). If Monday’s result is “no match,” execute calmly: refine your target list to programs aligned with your profile, customize PS quickly, and coordinate references for same-day calls. After SOAP, debrief—what truly limited interviews—and plan a 6–9-month upgrade (fresh USCE, targeted research, Step 3). Use this list during final review; check each item the week before ERAS submission and again after your first interview block. Consistency—not intensity—wins.The 12-Month ECFMG→ERAS Roadmap (What to Do and When)
Window Milestones Evidence/Artifacts −12 to −9 mo Pick ECFMG Pathway; book OET; plan Step 2 CK; set up EPIC/ERAS tokens. Pathway checklist, OET booking, Step 2 CK date, verified IDs. −9 to −6 mo USCE/observership; identify letter writers; PS draft; case/story log. Attendance logs, letter invites, PS v1, outcomes bullets. −6 to −3 mo Take Step 2 CK (± Step 3); build program tiers; write signal blurbs. Score report, tiering sheet, 100-word program fit notes. −3 to −1 mo Finalize Pathway + OET; complete ERAS; pre-assign docs; test interview tech. ECFMG “complete” status, ERAS receipt confirmations, tech checklist. Scores & Signals: Converting Your Profile into a Specialty Strategy
USCE That Converts: From Observerships to Credible, Specific Letters
Master your USMLE prep with MDSteps.
100+ new students last month.
Build an ERAS That Survives 30-Second Screens
Preference Signaling & Tiering: A Simple, Data-Savvy Allocation
Interview Playbook for IMGs: Clear, Concise, and Culturally Fluent
From Interview to Rank: Ethical Follow-Up, Notes, and Risk Management
Rapid-Review Checklist (T-30 to T-0 Days)
Eligibility & Documents
Signals & Communication
Interview Day Essentials
Common IMG Pitfalls—and How to Avoid Them
Sources & Further Reading
IMG to Match: ECFMG Timeline, Signals, and Interview Playbook