A practical, exam-day toolkit to decide whether to image, which modality, and how to spot the radiographic tells that board vignettes rely on.
First Principles: When to Image and What You Expect to Learn
Imaging is a decision, not a reflex. On exams, you earn points by matching modality to the question you need answered. Use this three-step script: (1) Rule out danger (fracture, dislocation, infection, cancer, neuro compromise); (2) Change management (is the result likely to alter immediate treatment?); (3) Minimize harm (radiation, contrast, cost, delay). For acute extremity trauma with focal bony tenderness or deformity, start with plain radiographs in two orthogonal views; add joint-above/below when indicated. Soft-tissue or occult injuries (e.g., rotator cuff tear, ligament injury, stress fracture) are MRI territory; tendon tears near skin may be ultrasound-friendly.
Don’t image routine low back pain within 6 weeks absent red flags (fever, neurologic deficit, cancer, trauma, weight loss). Severe or progressive deficits, suspected cauda equina, or infection → emergent MRI. Suspected osteomyelitis: MRI is early sensitive; X-ray lags by 1–2 weeks. For suspected septic arthritis, imaging is supportive; aspiration is diagnostic and therapeutic.
Decision Tools: Ottawa Rules and Clinical Gatekeepers
Decision rules save radiation and time. Ottawa ankle and foot rules recommend radiography for malleolar or midfoot pain with: bone tenderness at posterior edge/tip of malleoli, navicular, or base of 5th metatarsal, or inability to bear weight both immediately and in the clinic. Ottawa knee triggers X-ray after trauma if age ≥55, isolated patellar tenderness, fibular head tenderness, inability to flex to 90°, or inability to bear weight for 4 steps immediately and in the ED. Use them to justify imaging choices in stems.
| Presentation | Rule | Order X-ray? | Why |
|---|
| Ankle inversion injury, can’t bear weight | Ottawa Ankle | Yes | Functional inability → fracture risk |
| Midfoot pain, navicular tenderness | Ottawa Foot | Yes | High-risk bone |
| Twisted knee, age 30, full weight bearing | Ottawa Knee | No | No criteria met — consider soft-tissue injury |
Remember that rules are highly sensitive; a positive rule supports imaging, while a negative rule safely avoids it in low-risk patients. Persistent pain despite negative initial films merits re-evaluation or advanced imaging (e.g., navicular/scaphoid occult fractures).
Fracture Patterns and Classifications You Must Recognize
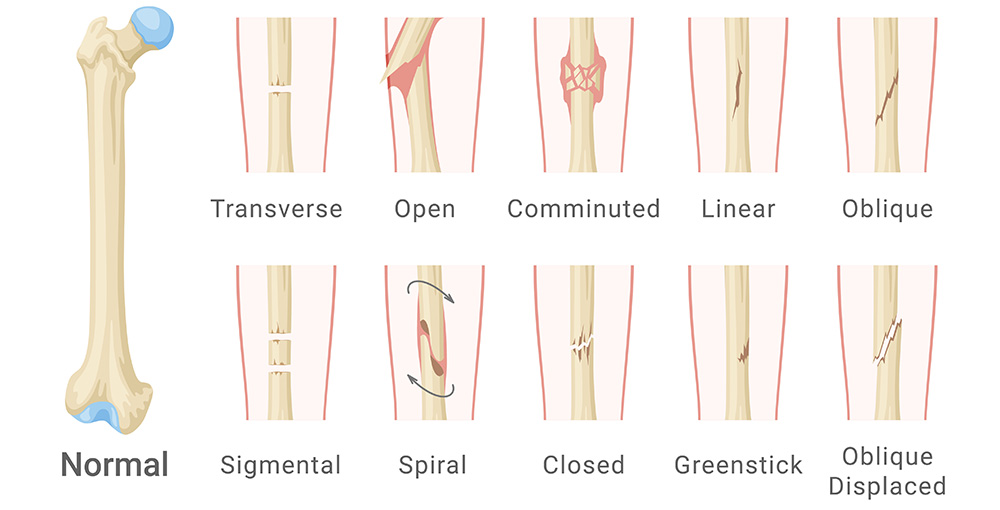
Examiners love eponyms and growth-plate logic. Salter-Harris (I–V) ranks physeal injuries by involvement: I (physis only), II (physis + metaphysis), III (physis + epiphysis), IV (all three), V (crush). Higher grade → greater growth disturbance risk. Scaphoid fractures present with snuffbox tenderness; initial radiographs can be normal—thumb spica plus MRI or repeat films in 10–14 days. Colles fracture (dorsal angulated distal radius) follows FOOSH; Smith is the volar variant. Jones fracture at the metaphyseal–diaphyseal junction of the 5th metatarsal heals poorly; avoid early weight bearing.
- Buckle (torus): Cortical bulge in children; stable; treat with short immobilization.
- Greenstick: Incomplete fracture in pediatrics; remodels well but may need reduction.
- Stress fracture: Insidious pain; early X-ray normal; MRI/bone scan positive.
On exams, pair the pattern with management intensity: intra-articular or displaced physeal injuries → ortho consultation; stable buckle fractures → simple immobilization and brief follow-up.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
Shoulder, Hip, and Elbow: Dislocation and Reduction Essentials
Anterior shoulder dislocation is most common—arm abducted and externally rotated; check axillary nerve sensation (lateral deltoid) before and after reduction. Posterior shoulder dislocation appears after seizure or electrocution; look for internal rotation, light-bulb sign, and difficulty with external rotation—commonly missed on AP view; request axillary or scapular Y-view. Posterior hip dislocation (dashboard injury) shortens and internally rotates the limb; emergent reduction protects femoral head blood supply—order AP pelvis and cross-table lateral; evaluate for acetabular fracture. Nursemaid’s elbow (radial head subluxation) in toddlers presents with pronated, flexed arm; radiographs often not required—perform hyperpronation or supination–flexion reduction and confirm return to use.
Always recheck neurovascular status after reduction and immobilize appropriately. Exams reward picking the imaging view that unveils the diagnosis: axillary view for posterior shoulder, frog-leg lateral for SCFE suspicion (though avoid if unstable slip).
Soft Tissue and Sports Imaging: Ultrasound vs. MRI
For tendons near the skin (Achilles, patellar, rotator cuff), ultrasound can rapidly differentiate partial vs. full-thickness tears and guide injections—with dynamic assessment under stress. MRI excels at intra-articular structures (menisci, cruciates, labrum), bone marrow edema (occult fracture, osteonecrosis), and infection extent. Use the clinical question to choose: suspected ACL tear after positive Lachman and effusion → MRI for surgical planning; suspected plantar fasciitis → no imaging initially; Achilles rupture with positive Thompson test → often clinical, US if needed.
- Bursa vs. joint effusion: US distinguishes superficial collections and guides aspiration.
- Dynamic entrapment: US during movement (snapping hip, peroneal subluxation).
- Hardware or contraindication to MRI: US or CT arthrography as alternatives.
When stems include resource constraints or pregnancy, ultrasound becomes a high-value, radiation-free first choice for many superficial MSK problems.
Radiographic Tells: The Subtle Signs Examiners Love
- Anterior/posterior fat pad sign (elbow): Occult supracondylar fracture in children; treat as fracture and immobilize.
- Lipohemarthrosis: Fat–fluid level suggests intra-articular fracture (e.g., tibial plateau); CT clarifies.
- Periosteal reaction patterns: Onion-skin (Ewing), sunburst/Codman triangle (osteosarcoma) — consider age and site.
- Sclerotic serpiginous lines: Osteonecrosis; MRI more sensitive early.
- Spondylolysis “collar on Scotty dog”: Pars interarticularis defect on oblique lumbar films; MRI/SPECT if needed.
Memorize these visual anchors and connect them to age and mechanism. If a stem hints at malignancy or infection, escalate to MRI/CT and labs rather than repeating plain films.
Complaint → Modality Matrix: Fast, Safe Choices
| Complaint | Red Flags? | First Test | If Negative but Suspicion High | Why |
|---|
| Acute ankle pain after inversion | Inability to bear weight | X-ray (Ottawa) | MRI for ligament/stress fracture | Rule out fracture; assess soft tissue if persistent |
| Snuffbox tenderness post-FOOSH | Yes—high-risk bone | X-ray + thumb spica | MRI or repeat X-ray 10–14 d | Vascular watershed; avoid nonunion |
| Low back pain, no neuro deficits | No | No imaging | MRI if >6 wk or deficits emerge | Reduce harm; low yield early |
| Hot, swollen knee | Yes (infection) | Arthrocentesis | US if unsure of effusion; MRI if osteomyelitis suspected | Fluids guide therapy; imaging is adjunct |
| Shoulder after seizure | Posterior dislocation risk | AP + axillary/Y view | CT if complex fracture-dislocation | Posterior missed on AP alone |
Use this matrix to choose imaging that answers the key clinical question while minimizing risk. If imaging won’t change management immediately, defer and reassess.
Rapid-Review Checklist: Imaging Pitfalls to Avoid
- Do not image routine low back pain within 6 weeks without red flags.
- Always obtain orthogonal views; request special views (axillary/Y) when dislocation suspected.
- Immobilize suspected scaphoid even if initial films are negative.
- Use MRI early for suspected osteomyelitis or stress fracture when X-rays are normal.
- Hot joint? Aspirate first—don’t delay for imaging.
- Reassess neurovascular status before and after reductions/splints.
If uncertain on a vignette, pick the option that best protects function and life (immobilize, aspirate, urgent MRI) rather than the most “interesting” image.
100+ new students last month.