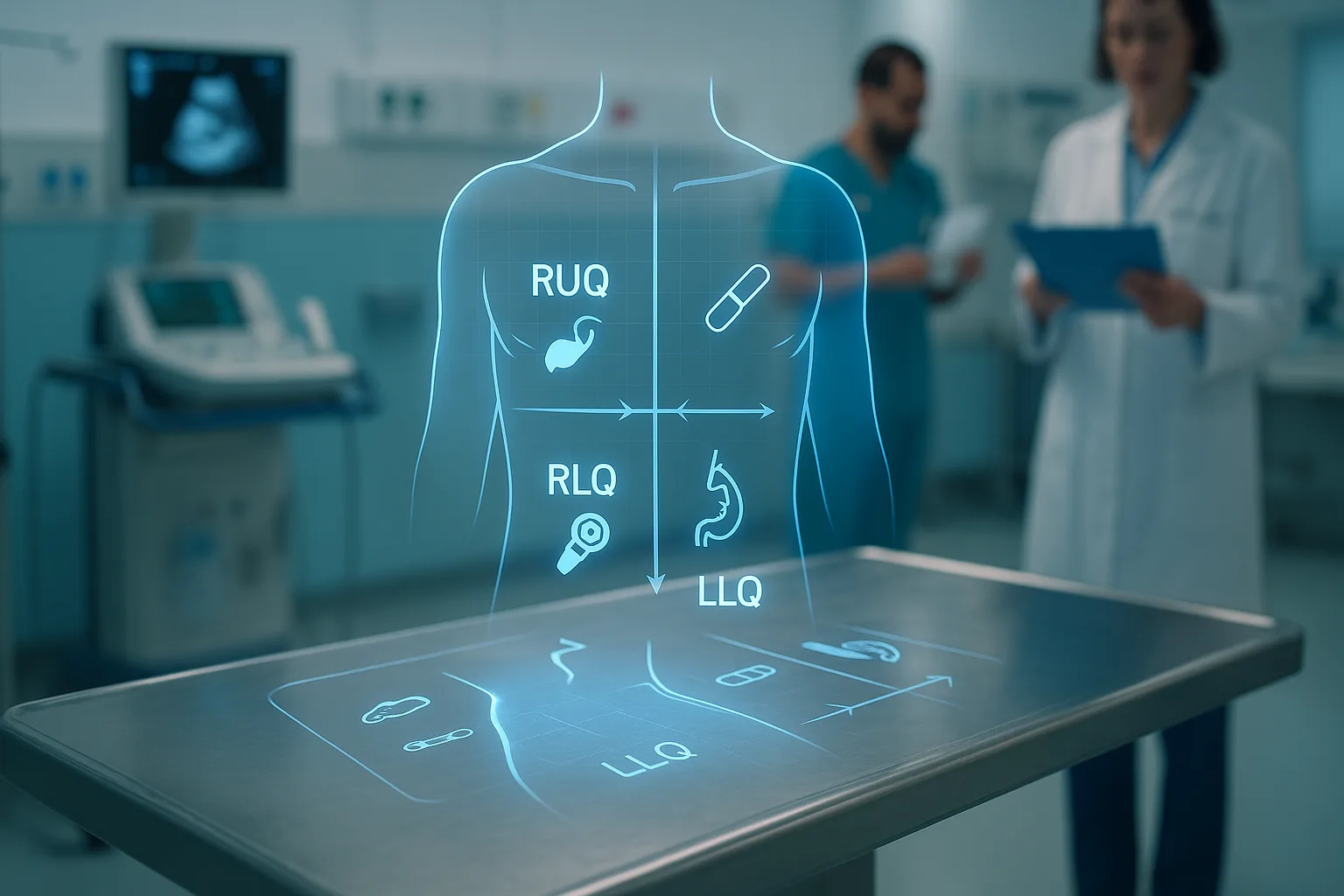
High-Yield Abdominal Pain Algorithms for the USMLE: RUQ, RLQ, LLQ Diagnostic Guide
Understanding How the USMLE Tests Abdominal Pain
Abdominal pain appears across Step 1, Step 2 CK, and Step 3, making it one of the highest-yield systems to master. The USMLE abdominal pain algorithm provides a structured approach to stabilize the patient, identify red flags, and rapidly narrow the differential using quadrant-based logic. Early in the vignette, the question stem typically provides clues related to pain location, onset, triggers, pregnancy status, recent operations, and key lab abnormalities. Your job is to identify which clues matter, eliminate distractors, and apply physiology-anchored decision-making.
Across Steps, the testing emphasis differs: Step 1 focuses on mechanisms (e.g., why biliary colic develops after fatty meals), Step 2 CK emphasizes diagnosis (e.g., differentiating appendicitis from ovarian torsion), and Step 3 involves management prioritization (e.g., ordering RUQ ultrasound for suspected cholecystitis). A recurring challenge is the exam’s preference for incomplete data; you must decide the next best diagnostic or treatment step rather than arrive at a final diagnosis.
Quadrant-based evaluation is therefore essential. RUQ pain often reflects hepatobiliary pathology; RLQ pain frequently involves appendiceal or gynecologic disease; LLQ pain classically suggests diverticulitis. However, the USMLE tests exceptions deliberately—right-sided diverticulitis, atypical appendicitis, and pregnancy-related organ displacement. Good question takers use decision trees rather than memorized lists, which is why algorithmic thinking is rewarded.
Below is a compact summary of quadrant-triggering clues commonly embedded in vignettes:
| Quadrant | High-Yield USMLE Clues |
|---|
| RUQ | Fever + ↑WBC; ↑ALP/↑GGT; Murphy sign; postprandial pain; jaundice |
| RLQ | Migratory pain; anorexia; pregnancy; sudden severe pain in reproductive-age women |
| LLQ | Older patient; fever; change in bowel habits; chronic constipation |
Throughout this guide, you will see algorithm boxes, exam traps, physiologic reasoning, and red flags. MDSteps’ adaptive QBank (9000+ questions) mirrors these patterns by clustering abdominal scenarios according to quadrant and integrating timed diagnostic decision-making, similar to NBME logic.
RUQ Pain: Hepatobiliary and Pulmonary Algorithms
RUQ pain on the USMLE typically highlights gallbladder disease, hepatic inflammation, or referred pulmonary pathology. Early recognition of severity matters: cholangitis and acute cholecystitis require urgent intervention, whereas biliary colic is usually mild and transient. Start by identifying systemic features—high fever, hypotension, jaundice, or altered mental status all signal dangerous disease such as ascending cholangitis.
Algorithm for RUQ Pain (USMLE-Oriented):
Step 1: Assess red flags — fever, jaundice, hypotension, confusion, RUQ rebound tenderness.
Step 2: Order initial labs — CBC, CMP, lipase, LFT pattern recognition (cholestatic vs hepatocellular).
Step 3: Choose first-line imaging — RUQ ultrasound (always first for gallbladder disease).
Step 4: Branch by imaging
- Thickened wall + pericholecystic fluid → Acute cholecystitis
- Dilated CBD + jaundice → Choledocholithiasis (MRCP/ERCP)
- Fever + hypotension + jaundice → Ascending cholangitis (ERCP urgently)
- Normal US but pain after fatty meals → Biliary colic
Always remember the hepatic causes: viral hepatitis produces RUQ discomfort with markedly elevated AST/ALT proportional to hepatocellular damage. Alcoholic hepatitis reveals AST:ALT ratio >2. The USMLE likes to differentiate these conditions by the presence or absence of jaundice, alcohol history, and transaminase patterns.
Pulmonary causes such as right lower-lobe pneumonia can mimic RUQ pain. Count on NBME to hide the cough or fever early in the vignette; dullness to percussion or crackles are usually clues. Diaphragmatic irritation explains the referral, and CXR becomes the appropriate next test.
MDSteps’ QBank intentionally mixes biliary and pulmonary vignettes to train pattern recognition and prevent premature closure—one of the most common cognitive traps with RUQ presentations.
RLQ Pain: Appendicitis, Gynecologic Emergencies, and Urologic Conditions
The RLQ contains the most commonly tested abdominal emergency: appendicitis. However, the USMLE frequently disguises appendicitis by altering onset or order of symptoms, such as presenting vomiting before pain or mimicking urinary symptoms. A strong USMLE abdominal pain algorithm must therefore branch early into gynecologic and urinary differentials, especially in reproductive-age women.
RLQ Algorithm (Exam-Focused)
- Step 1: Pregnancy test in all reproductive-age women
- Step 2: Stabilize if hypotensive or febrile
- Step 3: Characterize pain — migratory? sudden? constant?
- Step 4: Branch
- Migratory periumbilical → RLQ + anorexia: Appendicitis → US (kids) or CT (adults)
- Sudden severe unilateral pelvic pain: Ovarian torsion → Pelvic US with Doppler
- Dysuria, hematuria: Ureteral stone → CT KUB
- Pregnancy + bleeding or hypotension: Ectopic → Transvaginal US
Appendicitis management depends on imaging. In adults, CT abdomen with contrast is preferred. In children or pregnant patients, ultrasound is first-line. Do not be tricked by “nonvisualized appendix”—look for supportive secondary signs such as fat stranding, free fluid, or dilated tubular structure.
Gynecologic emergencies appear frequently on Step 2 CK and Step 3. Torsion classically presents with sudden pain and nausea without fever or leukocytosis. Pelvic inflammatory disease (PID) presents with cervical motion tenderness, mucopurulent discharge, and bilateral pelvic pain. Ectopic pregnancy is always ruled out first in pregnant patients.
Renal colic is another distractor. Colicky flank pain radiating to the groin with hematuria and costovertebral angle tenderness points to a ureteral stone. Proceed to CT KUB unless the patient is pregnant, where ultrasound becomes first-line.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
LLQ Pain: Diverticulitis, Colitis, and Vascular Emergencies
LLQ pain is most commonly diverticulitis, especially in older adults with fever and leukocytosis. The USMLE tests whether you can differentiate uncomplicated diverticulitis (managed with oral antibiotics as outpatient) from complicated disease (abscess, perforation, fistula, obstruction). CT abdomen with contrast is the diagnostic gold standard and will show fat stranding or abscess formation.
If the vignette mentions severe pain out of proportion to exam findings—in elderly patients with atrial fibrillation—consider mesenteric ischemia. LLQ ischemia (ischemic colitis) may present with crampy pain and bloody diarrhea. This distinction is critical because the former is a surgical emergency while the latter is managed with supportive care.
Inflammatory bowel disease is another LLQ mimic. Chronic diarrhea, weight loss, and extraintestinal manifestations such as uveitis or arthritis are clues. The USMLE may hide these features initially, but colonoscopy is ultimately required for diagnosis. Volvulus, especially sigmoid volvulus, presents with abdominal distention, constipation, and “coffee bean” sign on X-ray. Endoscopic detorsion is first-line unless perforation is suspected.
Because LLQ pathology often overlaps, your decision-making must integrate systemic symptoms (fever, bleeding), onset pattern (sudden vs progressive), and risk factors (AFib, chronic constipation, prior colonoscopy). Keeping the LLQ flow structure clear allows rapid vignette navigation.
Cross-Quadrant Emergencies: AAA, Mesenteric Ischemia, and Pancreatitis
Some life-threatening conditions transcend quadrants and appear throughout USMLE exams: abdominal aortic aneurysm, mesenteric ischemia, acute pancreatitis, spontaneous bacterial peritonitis, and perforated viscus. Recognizing these early saves time and avoids distractors designed to lure you toward benign diagnoses.
AAA typically manifests as back or abdominal pain with hypotension in older men with a smoking history. The key next step is bedside ultrasound if unstable, or CT angiography if stable. Mesenteric ischemia produces pain “out of proportion” to physical findings and may feature sudden onset after arrhythmia or embolic event. Serum lactate is often elevated, but CT angiography is the diagnostic test of choice.
Pancreatitis shows epigastric pain radiating to the back with elevated lipase. The USMLE often tests the difference between gallstone and alcohol-induced pancreatitis. Ranson criteria or BISAP may appear when assessing severity. CT scan is not needed for initial diagnosis but becomes relevant when the clinical course worsens or necrosis is suspected.
Spontaneous bacterial peritonitis (SBP) appears in cirrhotic patients with ascites who develop diffuse pain, fever, or encephalopathy. Diagnosed via paracentesis showing neutrophils ≥250 cells/µL. Perforated ulcers cause sudden severe generalized pain with free air under the diaphragm on upright chest X-ray, requiring emergent surgical intervention.
Cross-quadrant emergencies require rapid stabilization—fluids, oxygen, and sometimes antibiotics—before imaging. Step 3 in particular evaluates prioritization: stabilize first, then image.
Imaging Decision-Making on the USMLE
The USMLE tests correct imaging selection heavily. Choosing the wrong modality—even if it eventually leads to the correct diagnosis—results in a missed question. The correct initial studies depend on quadrant, reproductive status, and hemodynamics. Below is a compact imaging guide.
| Condition | Imaging |
|---|
| Cholecystitis | RUQ ultrasound |
| Choledocholithiasis | MRCP → ERCP |
| Appendicitis (adult) | CT abdomen with contrast |
| Appendicitis (child/pregnancy) | Ultrasound first-line |
| Nephrolithiasis | CT KUB (noncontrast) |
| Ectopic pregnancy | Transvaginal ultrasound |
| Diverticulitis | CT abdomen with contrast |
| AAA (unstable) | Bedside ultrasound |
The decision tree is straightforward: choose the least invasive test that yields the highest diagnostic value without delaying care. For Step 3, the presence of hemodynamic instability shifts imaging choices toward bedside options.
Common USMLE Traps, Errors, and Cognitive Biases
Many abdominal pain errors stem from cognitive biases. Anchoring on a single symptom can lead to missing more serious conditions. Premature closure—committing to a diagnosis before sufficient data—is a classic pitfall, especially in RUQ and RLQ pain where symptoms overlap. Availability bias appears when a student over-calls appendicitis simply because it is common on exams.
To avoid these traps, use algorithmic reasoning: stabilize, rule out life-threatening conditions, branch by quadrant, and choose imaging deliberately. Exam stems often bury critical clues in subtle descriptors. For example, “vomiting before pain” helps differentiate ovarian torsion from appendicitis, and “pain worse after meals” suggests mesenteric ischemia in elderly patients.
MDSteps’ analytics dashboard highlights your missed patterns and automatically generates flashcards to reinforce the clues you tend to overlook—avoiding repetition of these errors during full-length practice exams.
Rapid-Review Checklist
- RUQ pain → start with RUQ ultrasound
- RLQ pain in women → pregnancy test first
- LLQ pain + fever → diverticulitis → CT with contrast
- Pain out of proportion → mesenteric ischemia
- Hypotension + back pain → AAA → bedside ultrasound
- Epigastric pain radiating to back → pancreatitis → lipase
- Unstable patients → stabilize before imaging
- Never order CT for biliary disease first-line
- Use Doppler ultrasound for suspected torsion
- Always consider atypical presentations
Medically reviewed by: Jonathan Reyes, MD – Internal Medicine
References
100+ new students last month.