Anatomy → Function → Predictable Clinical Patterns
Boards reward rapid translation of anatomy into “illness scripts”—compact, testable stories that connect mechanism, key findings, and the next best step. Build your MSK core around three ladders: (1) motion unit (bone–joint–muscle–nerve), (2) load & failure (how tissue fails and how it presents), and (3) triage (red flags first). Start proximally and move distally. For each region, identify the prime movers, innervation, vascular supply, and stabilizers, then attach high-yield injuries and maneuvers. Example: the rotator cuff centers glenohumeral stability; supraspinatus initiates abduction (C5, suprascapular nerve). Painful arc and positive empty-can suggests supraspinatus pathology; weakness after fall on outstretched hand (FOOSH) favors tear—next best imaging often MRI if surgical planning is anticipated.
| Structure | Function | Classic Presentation | High-Yield Test | Next Best Step |
|---|
| Radial nerve (spiral groove) | Wrist/finger extensors | “Saturday night palsy,” wrist drop | Sensory dorsum 1st web space; resisted extension | Splint, avoid pressure; r/o humeral shaft fracture |
| Ulnar nerve (cubital tunnel) | Interossei, adductor pollicis | Numb 4th/5th digits, intrinsic hand weakness | Froment sign, Wartenberg sign | Activity modification; consider nerve conduction |
| Supraspinatus tendon | Abduction initiation | Lateral shoulder pain, night pain | Empty-can, painful arc | Activity + PT; MRI if trauma/weakness > surgical eval |
| ACL | Anterior tibial restraint | Pop + swelling after pivot | Lachman (> Anterior drawer) | Brace + MRI; ortho referral |
As you study, convert each row into a flashcard that prompts for mechanism, exam maneuver, and disposition. Rehearse with time pressure: read the stem, identify the ladder (motion unit → load → triage), and pick the single next action that minimizes morbidity (immobilize, image, aspirate, or reassure).
Nerve Lesions, Dermatomes, and Myotomes—Fast Localization
Localization collapses MSK neurology into a few anchors. Think “root → plexus → named nerve” and test both sensory territory and a single myotome movement. Cervical myotomes: C5 (shoulder abduction), C6 (elbow flexion/wrist extension), C7 (elbow extension/wrist flexion), C8 (finger flexion), T1 (interossei). Dermatomal pain down the arm or leg with reflex changes suggests radiculopathy; isolated motor/sensory deficits in a peripheral nerve territory suggests mononeuropathy. Boards love distinguishing C7 radiculopathy (triceps weakness, ↓ triceps reflex) from radial neuropathy (wrist/finger extension weakness, sensory dorsal hand).
- Upper limb traps: Spiral groove compression (radial), surgical neck (axillary deltoid weakness), medial epicondyle injury (ulnar claw).
- Lower limb anchors: L4 (knee extension, patellar reflex), L5 (dorsiflexion, heel walk), S1 (plantarflexion, Achilles reflex). Peroneal nerve palsy causes foot drop with dorsal foot numbness; tibial neuropathy impairs plantarflexion and sole sensation.
- Provocation tests: Phalen/Tinel (median at carpal tunnel), Finkelstein (De Quervain), Tinel at fibular neck (peroneal).
Exam stems often embed load or posture (crutches compressing axilla → posterior cord/radial issues). When localization is in doubt, “test one root and one nerve” approach: pick a myotome movement and a cutaneous patch that uniquely separates two contenders. Management emphasizes activity modification, splinting to protect function (e.g., wrist splint for radial palsy), and red flags (rapidly progressive weakness, sphincter signs → urgent imaging).
Tendons, Ligaments, and Region-Based Maneuvers
Muscle/tendon and ligament injuries follow predictable mechanisms. Overhead activity provokes rotator cuff tendinopathy; axial load + valgus stress injures MCL; sudden deceleration with pivoting tears the ACL. Exam maneuvers pair with anatomy and are frequently the single best next step in the stem.
Shoulder
- Impingement/tendinopathy: Neer/Hawkins; treat with activity change, PT, NSAIDs.
- RC tear: Weakness on empty-can/external rotation after trauma; MRI if surgical candidate.
- Adhesive capsulitis: Global stiffness > pain; diabetes risk; PT is cornerstone.
- Anterior dislocation: Abducted, externally rotated arm; check axillary nerve sensation.
Knee & Ankle
- ACL: Lachman (most sensitive). Rapid effusion within hours.
- PCL: Posterior drawer; dashboard injury.
- Meniscus: Joint line tenderness, Thessaly/McMurray; effusion develops more slowly.
- High-ankle (syndesmosis): External rotation + squeeze test; longer rehab.
On exam day, choose maneuvers that maximize separation between diagnoses (e.g., Lachman vs. anterior drawer). Early immobilization and protected weight bearing are low-risk decisions when severe injury is plausible; reserve advanced imaging for surgical planning or persistent deficits.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
Bone Biology, Infection, and Metabolic Themes
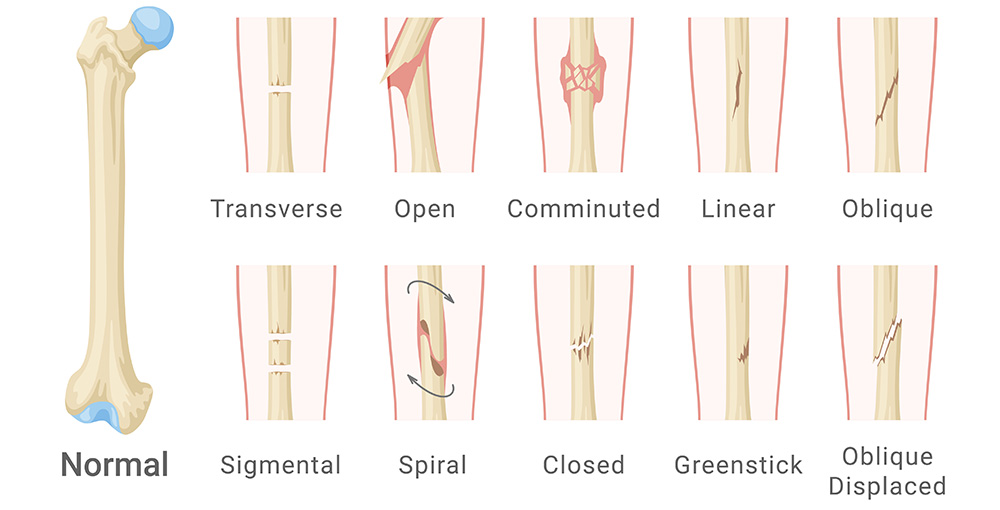
Understanding bone remodeling clarifies fractures and metabolic conditions. Osteoclast-mediated resorption and osteoblast formation are coupled by RANKL/OPG signaling. Pathology stems from imbalance: osteoporosis (reduced bone mass, normal mineralization), osteomalacia/rickets (defective mineralization, low vitamin D), and osteitis fibrosa (hyperparathyroidism). Boards test risk recognition (steroids, menopause, immobility) and first-line therapies: weight-bearing exercise, calcium/vitamin D, and antiresorptives (bisphosphonates) for appropriate T-scores or fracture history.
For bone infection, osteomyelitis presents with fever, localized pain, elevated inflammatory markers; sickle cell disease favors Salmonella, otherwise Staph aureus. Early X-rays can be normal; MRI is sensitive. Management is early empiric antibiotics tailored to organism; surgical debridement for abscess or hardware infection. Don’t miss septic arthritis: hot, swollen joint, decreased ROM—aspirate before antibiotics when feasible; synovial WBC often >50,000 with neutrophil predominance.
Fragility fractures (vertebral compression, hip) signal systemic disease. Use FRAX and DEXA-guided thresholds for therapy. In pediatrics, distinguish physeal (Salter-Harris) injury from normal variants; in elderly, low-energy hip fractures need prompt surgery and DVT prophylaxis. Tie bone biology back to management choices—for instance, why bisphosphonates reduce vertebral fractures (antiresorptive) yet atypical femur fracture risk rises with long-term use (oversuppressed remodeling).
Inflammatory vs. Mechanical: Building Fast Illness Scripts
Rapid triage depends on pattern recognition. Inflammatory pain: morning stiffness >60 minutes, improves with activity, swollen/warm joints, high ESR/CRP; think RA, spondyloarthropathy, crystalline disease, infection. Mechanical pain: worsens with use, brief morning stiffness, focal tenderness (tendinopathy, OA, bursitis). Use distribution and time course to shortcut differentials:
- Acute monoarthritis: Rule out septic arthritis first (fever, inability to bear weight). Aspirate—send Gram stain, culture, crystals.
- Symmetric small joints >6 weeks: RA. Order RF and anti-CCP; start NSAIDs/steroids short term and refer for DMARDs.
- Back pain with alternating buttock pain, morning stiffness, young adult: Axial spondyloarthritis; check HLA-B27 if indicated; MRI sacroiliac joints for early disease.
- First MTP, sudden nighttime pain: Gout; needle-shaped, negatively birefringent crystals; treat with NSAID, colchicine, or steroid depending on comorbids.
When stems force an immediate action, default to safety: aspirate the hot joint, immobilize suspected fracture/dislocation, and image when red flags exist. Use labs to confirm—not to delay—time-sensitive decisions.
Pharmacology Across Steps: Analgesia, Steroids, and DMARD Logic
Analgesic choices hinge on mechanism and risk. For acute sprain/strain without red flags, start acetaminophen and NSAIDs; avoid opioids except for short-course, severe trauma scenarios. Add topical NSAIDs for localized OA. Glucocorticoids are potent but carry metabolic and infection risks; prefer local injections for focal inflammatory conditions (e.g., trigger finger, bursitis) after excluding infection and fracture. Neuropathic pain (radiculopathy) may respond to gabapentinoids or TCAs; weigh sedation and misuse potential.
In inflammatory arthritis, short steroid tapers control flares while DMARDs (methotrexate first-line for RA) modify disease trajectory. Check pregnancy status, alcohol use, liver/kidney function, and give folate with methotrexate. Biologics target TNF, IL-6, or costimulation pathways; screen for TB and hepatitis B prior to initiation. Crystal disease flares are treated acutely with NSAIDs/colchicine/steroids; urate-lowering therapy (allopurinol) is preventive and continued during flares with prophylaxis.
Exam logic: choose the safest effective regimen that aligns with the suspected mechanism and the patient’s comorbidity profile (CKD limits NSAIDs, anticoagulation complicates injections). Recognize drug–disease pitfalls (fluoroquinolones → tendinopathy; bisphosphonates → esophagitis if recumbent dosing).
Practice Architecture: Qbanks, Retrieval, and a Weekly MSK Loop
Convert MSK into durable skills through spaced retrieval and case-based practice. Use a repeatable weekly loop: (1) two focused Qbank blocks (mixed MSK + systems), (2) brief error autopsy mapping each miss to anatomy/illness-script ladders, (3) targeted Anki on mechanisms and maneuvers, (4) one mini-assessment with timed questions.
| Day | Focus | Primary Task | Output |
|---|
| Mon | Upper limb | 40 mixed Qs + review | 3 cards: nerve, maneuver, dispo |
| Wed | Lower limb/spine | 40 mixed Qs + review | Flow for red flags vs. benign |
| Fri | Inflammatory vs mechanical | 20 timed Qs | Checklist: aspirate/image/immobilize |
| Sun | Imaging & emergencies | Image identification drill | Top 10 signs gallery |
Keep notes minimal and visual; prioritize tables and checklists you can rehearse under 60 seconds. The goal is fast pattern access, not encyclopedic recall.
Rapid-Review Checklist: Don’t Miss, Don’t Over-Treat
- Hot, immobile joint → aspirate before antibiotics (if stable).
- Trauma + deformity/neurologic deficit → reduce/immobilize and recheck pulses/sensation.
- Back pain + urinary retention/saddle anesthesia → emergent MRI (cauda equina).
- Night pain, constitutional symptoms, or persistent pain despite rest → image and labs.
- FOOSH with snuffbox tenderness → thumb spica + repeat imaging/MRI for occult scaphoid.
- Rapid compartment pain out of proportion + pain on passive stretch → emergent fasciotomy.
- RA diagnosis > start DMARD; steroids only bridge.
Use this list as your pre-exam warmup: if a stem triggers one of these, you likely know the correct “next step.”
100+ new students last month.