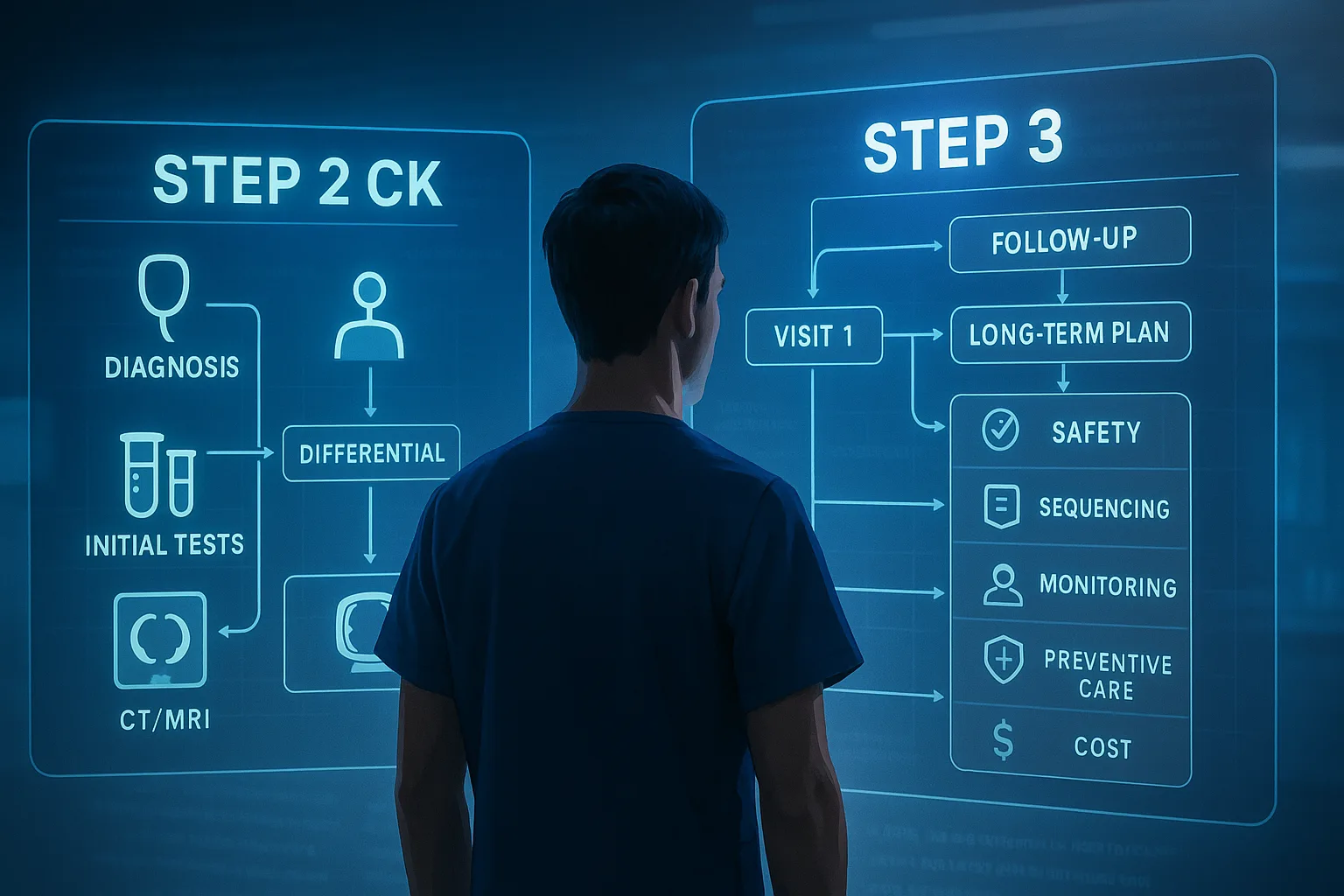
1) Orientation & Exam Strategy: Stabilize First, Decide Delivery Second
Step 3 vignettes on hypertensive disorders of pregnancy (HDP) reward a “stabilize → classify → deliver or defer” sequence. Stabilization is immediate whenever blood pressure (BP) is severe (systolic ≥160 or diastolic ≥110 mm Hg, persisting ~15 minutes): give an evidence-based antihypertensive rapidly (IV labetalol, IV hydralazine, or oral immediate-release nifedipine) to reduce maternal stroke risk while avoiding precipitous drops. Target is not normotension; bring BP into the 140–150/90–100 window to protect perfusion. In parallel, start seizure prophylaxis with magnesium sulfate (MgSO4) when severe features are present or if eclampsia has occurred, and arrange continuous maternal–fetal monitoring.
Classification determines delivery timing. Preeclampsia without severe features and gestational hypertension are usually delivered at ≥37 weeks; preeclampsia with severe features prompts delivery at ≥34 weeks once the mother is stabilized. Before 34 weeks, carefully selected, stable patients may be managed expectantly at tertiary centers with strict maternal–fetal surveillance; any maternal or fetal deterioration terminates expectant management. Do not delay an indicated delivery to complete corticosteroids if the gestational age is late preterm and disease is worsening.
Prototype vignette cues include persistent headache unresponsive to acetaminophen, visual phenomena, right-upper-quadrant/epigastric pain, dyspnea/pulmonary edema, oliguria, platelets <100,000/µL, creatinine >1.1 mg/dL or doubling baseline, elevated AST/ALT ≥2× normal, and sustained severe-range BP. The absence of proteinuria does not exclude preeclampsia if these end-organ findings exist. On exam day, the “next best step” after confirming severe BP is to treat within 30–60 minutes, draw labs (CBC, creatinine, AST/ALT, LDH), obtain urine protein/creatinine ratio, start MgSO4 when indicated, and determine the delivery plan based on gestational age and stability.
Common wrong answers: delaying treatment while repeating BP endlessly; using ACE inhibitors or nitroprusside antepartum; giving methylergonovine for postpartum atony in a hypertensive patient; chasing normal BPs with excessive medication; or skipping MgSO4 in a patient with severe features. The exam also probes postpartum disease—recognize that new-onset hypertension/eclampsia may occur after delivery and requires the same urgency in BP control and seizure prophylaxis.
2) Core Pathobiology: Abnormal Placentation, Endothelial Injury, Microangiopathy
Preeclampsia originates in abnormal placentation with shallow trophoblastic invasion and failure to remodel spiral arteries, producing a high-resistance uteroplacental bed. Placental ischemia triggers release of anti-angiogenic factors (e.g., sFlt-1) that neutralize VEGF/PlGF and cause systemic endothelial dysfunction. The maternal phenotype includes capillary leak (edema, pulmonary edema), vasospasm (hypertension, cerebral/visual symptoms), glomerular endotheliosis (proteinuria, rising creatinine), and microangiopathic hemolysis with consumptive thrombocytopenia in severe disease (HELLP). This mechanistic chain explains why proteinuria is neither necessary nor sufficient once end-organ injury is present.
Microangiopathic injury underlies HELLP (Hemolysis, Elevated Liver enzymes, Low Platelets). Classically, platelets <100,000/µL, AST ≥70 IU/L, and LDH ≥600 U/L define complete Tennessee criteria, though variants exist and hypertension/proteinuria may be absent in a minority. Clinically, RUQ/epigastric pain, nausea/vomiting, and malaise predominate; abrupt deterioration, DIC, and hepatic hematoma/rupture are feared complications. Recognize HELLP as an indication for delivery after maternal stabilization, regardless of gestational age, because maternal risk outweighs fetal benefit when the syndrome evolves.
Fetal consequences stem from uteroplacental insufficiency: growth restriction, oligohydramnios, abnormal Dopplers, and late decelerations. Hence, antenatal surveillance (NSTs, BPPs) and serial growth assessments are integral when expectant management is entertained. Maternal disease severity and gestational age—rather than proteinuria grade—drive timing of delivery. For Step 3 logic, connect symptoms to mechanism: flashes/scotomata → posterior reversible encephalopathy from endothelial injury; oliguria → renal vasospasm and reduced perfusion; pulmonary edema → capillary leak + diastolic dysfunction; thrombocytopenia → consumptive microangiopathy. These mechanistic links justify why stabilization with antihypertensives and MgSO4 precedes any decision about induction vs cesarean.
3) Diagnostic Framework: Definitions, Severe Features, and the Minimum Workup
Key definitions (ACOG): Gestational hypertension is new-onset BP ≥140/90 mm Hg after 20 weeks on two readings ≥4 hours apart. Preeclampsia is hypertension plus either proteinuria (≥300 mg/24 h or protein/creatinine ≥0.3) or end-organ dysfunction. “Severe features” include any of: platelets <100,000/µL; creatinine >1.1 mg/dL or doubling baseline; transaminases ≥2× normal or persistent RUQ/epigastric pain; pulmonary edema; new-onset cerebral or visual symptoms; or severe-range BP (≥160/110 mm Hg) sustained. Proteinuria is not required when end-organ features exist.
| Entity | Diagnostic anchors | Implications |
|---|
| Gestational HTN | ≥140/90 after 20 wks; no proteinuria/end-organ | Deliver at ≥37 wks |
| Preeclampsia (no severe features) | HTN + proteinuria or minimal end-organ findings | Deliver at ≥37 wks |
| Preeclampsia with severe features | Any severe feature (see text) | Deliver ≥34 wks once stabilized; expectant <34 only if strictly selected |
| HELLP | Hemolysis, AST/ALT ↑, platelets <100k | Indication for delivery after stabilization |
Minimum maternal workup: CBC with platelets, CMP (creatinine, AST/ALT), LDH, urine protein/creatinine ratio; consider uric acid locally. Evaluate for pulmonary edema and neurologic symptoms. Fetal assessment: NST/BPP, growth ultrasound, ± umbilical artery Doppler if growth-restricted. Severe features or nonreassuring testing bias toward delivery. On exam questions, repeating dipsticks is low-value; a protein/creatinine ratio ≥0.3 is sufficient to confirm proteinuria without a 24-hour collection.
Finally, remember mimics and overlaps (TTP/HUS, acute fatty liver of pregnancy, lupus flare). Marked hemolysis with schistocytes and neurologic changes out of proportion to hypertension should prompt hematology input for plasma exchange (TTP). But if the vignette provides classic severe-range BP plus RUQ pain and platelets 70,000/µL at 33 weeks, treat as severe preeclampsia/HELLP—stabilize, give MgSO4, control BP, and proceed to delivery.
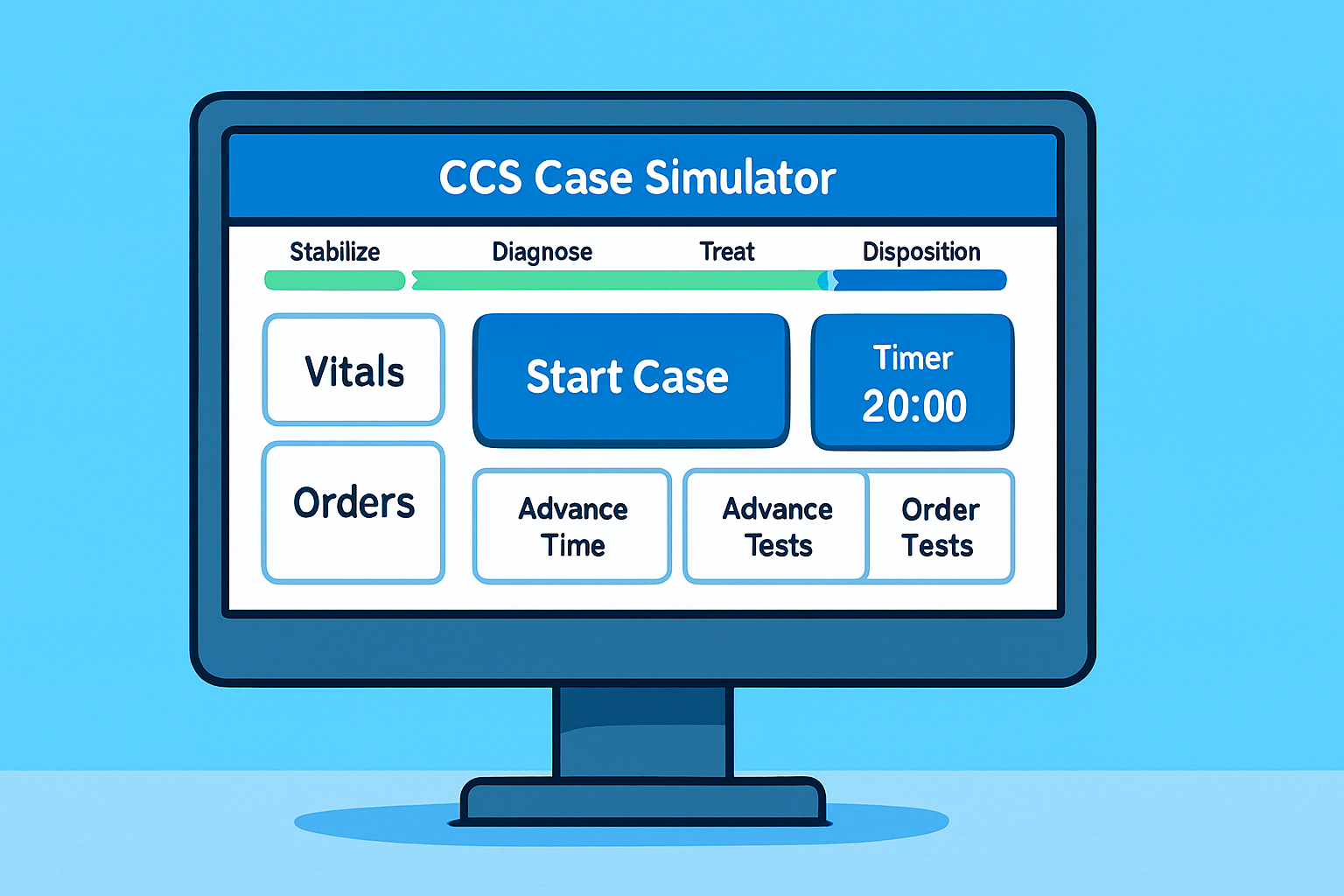
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
4) Acute BP Control: Drug Selection, Dosing, Targets, and Fluids
When to treat: acute-onset severe hypertension (SBP ≥160 and/or DBP ≥110 mm Hg) persisting about 15 minutes mandates treatment within 30–60 minutes to reduce maternal stroke risk. Targets: reduce into 140–150/90–100 mm Hg; avoid overshoot that compromises uteroplacental perfusion. Place IV access, continuous monitoring, restrict fluids to avoid pulmonary edema (often ≤80–100 mL/h unless bleeding), and assess urine output.
| Agent (first-line) | Initial dosing & escalation | Notes |
|---|
| IV labetalol | 10–20 mg IV → 20–80 mg q10–30 min (max 300 mg) or infusion 1–2 mg/min | Avoid in asthma, heart block, decomp HF; quick onset 1–2 min |
| IV hydralazine | 5–10 mg IV, repeat 5–10 mg in 20–40 min (max ~20 mg early; more per protocol) | Watch maternal hypotension and fetal decels |
| Oral IR nifedipine | 10 mg PO; if still ≥160/110 after 20–30 min, give 20 mg; may repeat 20 mg | Do not puncture capsules; effective when no IV access |
These regimens are endorsed in ACOG guidance and quality bundles. If one drug fails, switch classes (e.g., labetalol → hydralazine or nifedipine); obtain senior or MFM support for refractory cases. Nitroprusside is a salvage ICU drug because of potential fetal cyanide exposure; ACE inhibitors and ARBs are contraindicated antepartum. After initial control, transition to oral labetalol or nifedipine for maintenance.
Fluids/diuresis: preeclampsia is a leaky-capillary, low-oncotic state; excessive crystalloids invite pulmonary edema. Use judicious maintenance fluids and treat pulmonary edema with oxygen, diuretics, and BP control. Persistent oliguria after stabilization warrants cautious evaluation; avoid reflex fluid boluses unless bleeding or prerenal factors are clear.
5) Magnesium Sulfate: Who Gets It, How to Dose, and How to Monitor
Indications: MgSO4 is the drug of choice for seizure prophylaxis in preeclampsia with severe features and for treatment/prevention of recurrent seizures in eclampsia. It is not an antihypertensive. A standard U.S. regimen is a 4–6 g IV loading dose over 20–30 minutes followed by 1–2 g/h infusion, continued for 24 hours postpartum (or 24 hours after last seizure). If IV access is limited, 10 g IM (5 g in each buttock) can be used, followed by 5 g IM q4h. Begin the infusion before cesarean when indicated and continue intra- and postpartum.
Monitoring and toxicity: Track deep tendon reflexes, respiratory rate, and urine output; obtain serum levels if renal dysfunction or symptoms. Loss of patellar reflexes, respiratory depression, or new somnolence mandates stopping the infusion and giving 10 mL of 10% calcium gluconate (≈1 g) IV over 2–5 minutes, with ventilatory support as needed. Resume at a lower rate once safe. Magnesium potentiates nondepolarizing neuromuscular blockers; alert anesthesia pre-op.
| Scenario | Action | Pearls |
|---|
| Severe features antepartum | Start MgSO4 now; continue 24 h postpartum | Give before OR if cesarean planned |
| Eclampsia (seizure) | Load 6 g IV if not given; maintenance 2 g/h | Re-bolus 2–4 g for recurrent seizure |
| Renal impairment/oliguria | Lower rate; check levels; strict I&O | Toxicity risk ↑; keep calcium gluconate at bedside |
Debate persists about shortening postpartum magnesium in selected low-risk recoveries; however, authoritative guidance continues to recommend 24 hours postpartum, and exam logic follows that standard. If a vignette shows refractory seizures despite therapeutic magnesium, escalate temporarily with benzodiazepines and involve critical care.
6) Delivery Timing & Mode: When Stabilization Gives Way to Birth
General rules: Deliver at ≥37 weeks for gestational hypertension or preeclampsia without severe features. For preeclampsia with severe features, deliver at ≥34 weeks once the mother is stabilized. Before 34 weeks, expectant management is considered only for carefully selected, stable patients in high-resource centers with continuous maternal–fetal surveillance; any worsening (e.g., uncontrolled BP, nonreassuring testing, progressive thrombocytopenia, rising creatinine/LFTs, pulmonary edema, abruption, DIC, eclampsia) ends expectant care and triggers delivery.
| Clinical scenario | Timing | Notes |
|---|
| Gestational HTN or PEC (no severe features) | ≥37 wks | Induction favored; outpatient surveillance until then |
| PEC with severe features, stable | ≥34 wks | Stabilize (BP, MgSO4) then proceed |
| HELLP, eclampsia, abruption, nonreassuring fetus | Any GA | Deliver after maternal stabilization |
| PEC with severe features <34 wks, stable | Expectant with strict criteria | ICU-level surveillance; steroids; magnesium |
Mode of delivery: Vaginal delivery is preferred unless standard obstetric indications argue for cesarean (e.g., malpresentation, unfavorable cervix with urgent delivery, fetal status). At ≥34 weeks with severe features and an unfavorable cervix, induction with mechanical ripening and oxytocin is often attempted if time permits. Do not delay indicated delivery solely to finish a corticosteroid course in late preterm disease. The peridelivery plan should include MgSO4 continuation, careful fluid management, and anesthesia coordination (regional often feasible if platelets are adequate and patient is stable).
Special timing notes on superimposed preeclampsia (chronic HTN + new proteinuria or end-organ): without severe features, many are delivered at 37 weeks; with severe features, proceed at ≥34 weeks (or earlier for instability). The exam frequently tests that delivery is the only definitive therapy; antihypertensives and magnesium mitigate risk but do not cure the disease.
7) Special Situations: HELLP, Eclampsia, and the Postpartum Window
HELLP: Maternal risk (DIC, hepatic hematoma/rupture, renal failure) dominates the decision. After BP control and MgSO4, deliver regardless of gestational age. Transfuse platelets if urgently needed for cesarean or if severe thrombocytopenia with bleeding; coordinate with anesthesia for neuraxial candidacy. RUQ pain with rising AST/ALT and LDH >600 U/L should trigger immediate action.
Eclampsia: Prioritize airway/oxygenation, lateral positioning, and MgSO4 loading/maintenance. Control severe BP with first-line agents. Recurrent seizure after therapeutic magnesium can be treated with an additional 2–4 g MgSO4 bolus; refractory cases may need benzodiazepines and ICU care. Delivery follows stabilization, not during active convulsions.
Postpartum hypertension & preeclampsia: New-onset disease can occur days after delivery; anticipate an initial BP dip then a rise around 3–6 days postpartum. Treat severe BPs with the same urgency and start MgSO4 when severe features are present. For maintenance in lactating patients, nifedipine/amlodipine and labetalol are commonly used; ACE inhibitors (e.g., enalapril, captopril) are compatible with breastfeeding and effective postpartum. Arrange early BP checks (often within 72 hours and at 1–2 weeks) and counsel on long-term cardiovascular risk after any HDP.
| Postpartum meds (lactation) | Typical use | Notes |
|---|
| Labetalol | First-line oral maintenance | Low levels in milk; multiple daily dosing |
| Nifedipine/amlodipine | First-line oral maintenance | Once-daily options improve adherence |
| Enalapril/captopril | Postpartum only | Breastfeeding-compatible ACEIs |
8) Pitfalls & Rapid-Review: Board-Style Associations and Mini-Vignettes
Rapid-Review Checklist
- Severe BP (≥160/110) persisting ~15 min → treat within 30–60 min; target 140–150/90–100.
- Give MgSO4 for severe features or eclampsia; not an antihypertensive; continue 24 h postpartum.
- Delivery timing: ≥37 wks (no severe features); ≥34 wks (severe features once stabilized); earlier for HELLP/eclampsia/instability.
- HELLP (LDH ≥600, AST ≥70, platelets <100k) → deliver after stabilization.
- Postpartum: same severe BP thresholds; labetalol/nifedipine/enalapril are lactation-compatible.
Board-Style Associations
- Visual scotomata + severe BP → treat BP now, start MgSO4, plan delivery (age-based).
- RUQ pain + platelets 70k + AST 180 → HELLP; deliver after stabilization.
- Pulmonary edema after fluid boluses → diurese, control BP, MgSO4 if severe features.
- Postpartum day 4 severe headache + 170/112 → treat as hypertensive emergency and give MgSO4.
Mini-vignettes: (a) 28-year-old at 39 wks with 152/96, protein/creatinine 0.35, normal platelets—induce now (≥37 wks). (b) 31-year-old at 33+5 wks with 170/112, headache, platelets 95k—treat BP, start MgSO4, deliver after stabilization (no expectant management with HELLP). (c) Postpartum day 5 with 164/110 and visual changes—treat emergently; start MgSO4; begin nifedipine ER and arrange close follow-up.
100+ new students last month.