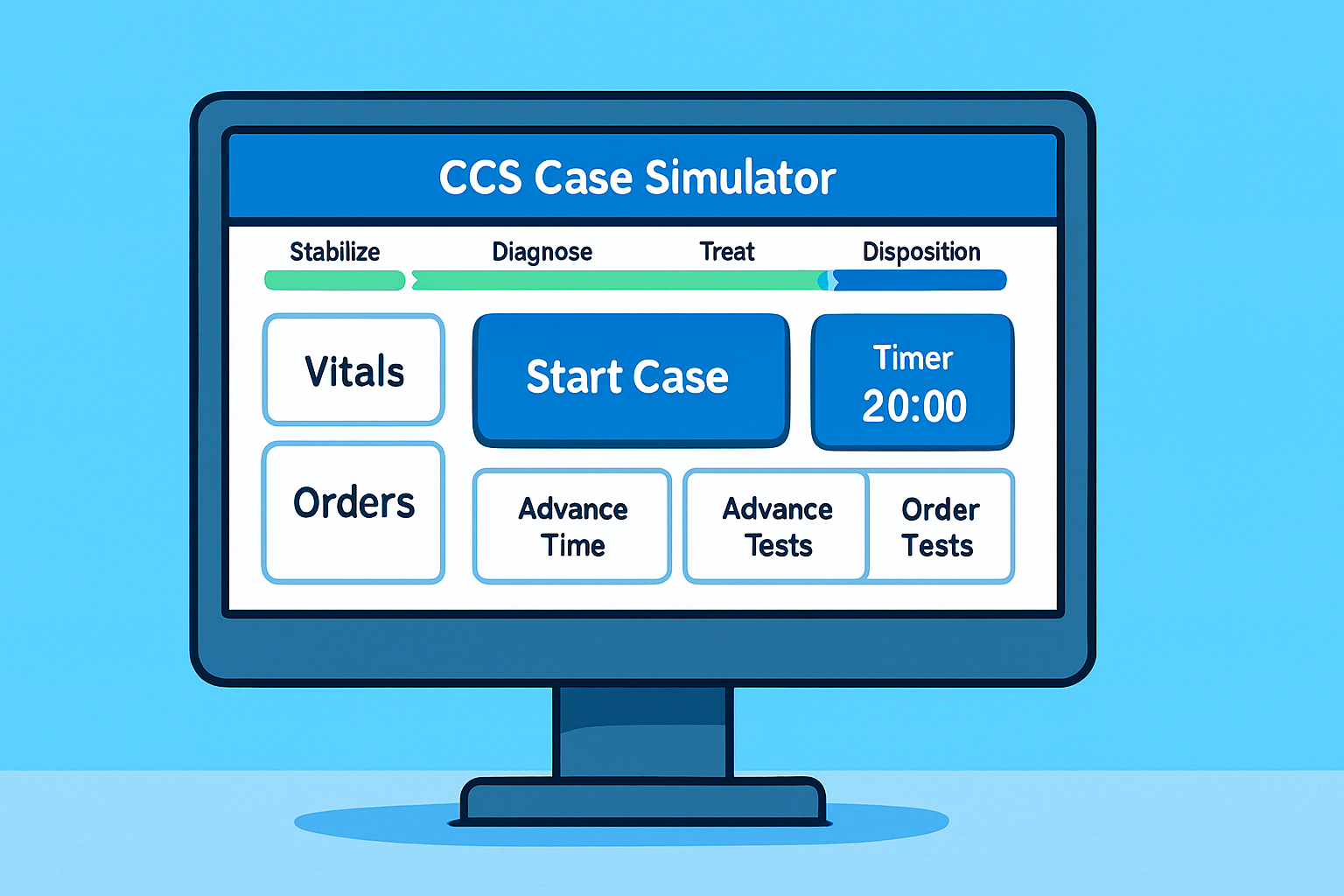
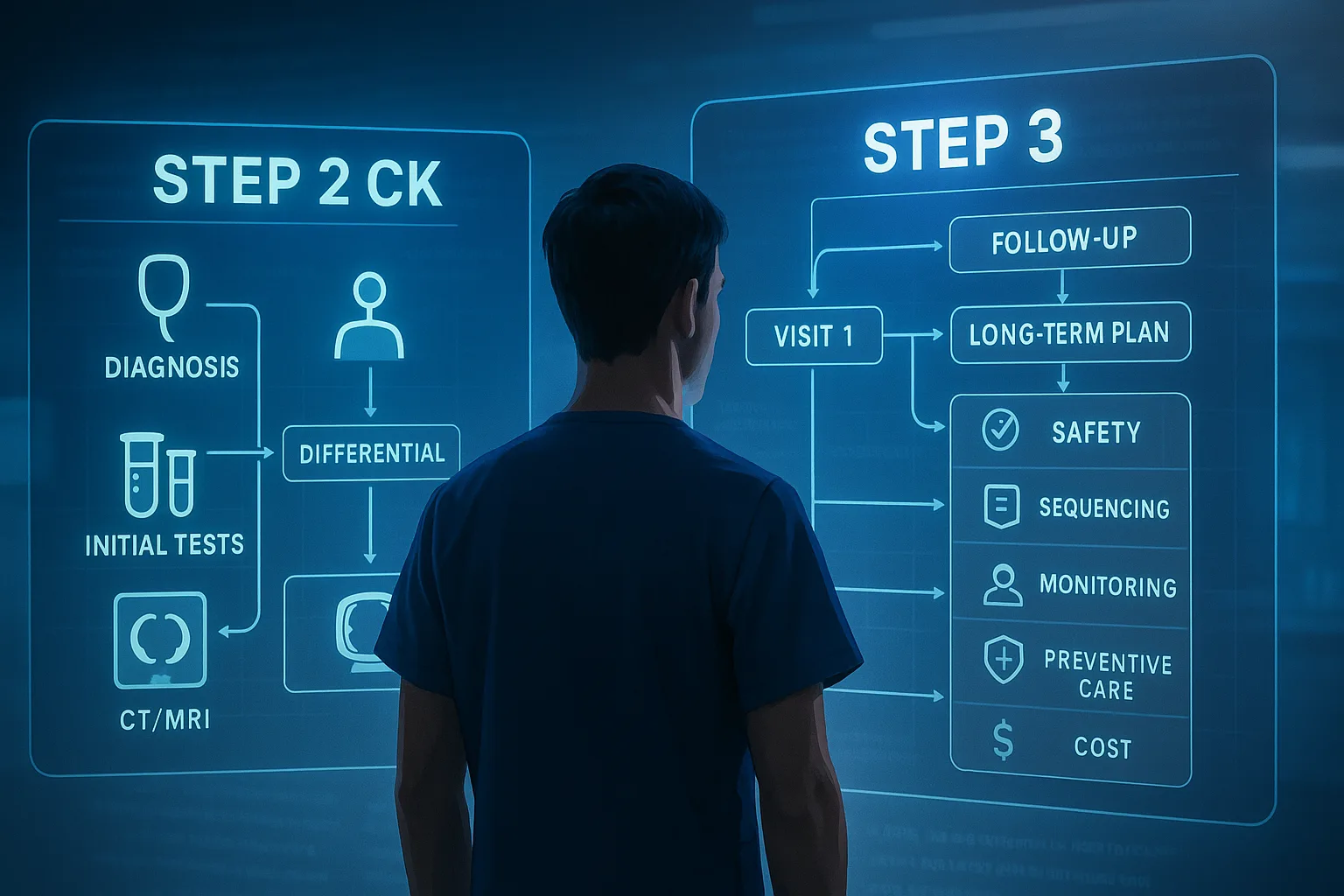
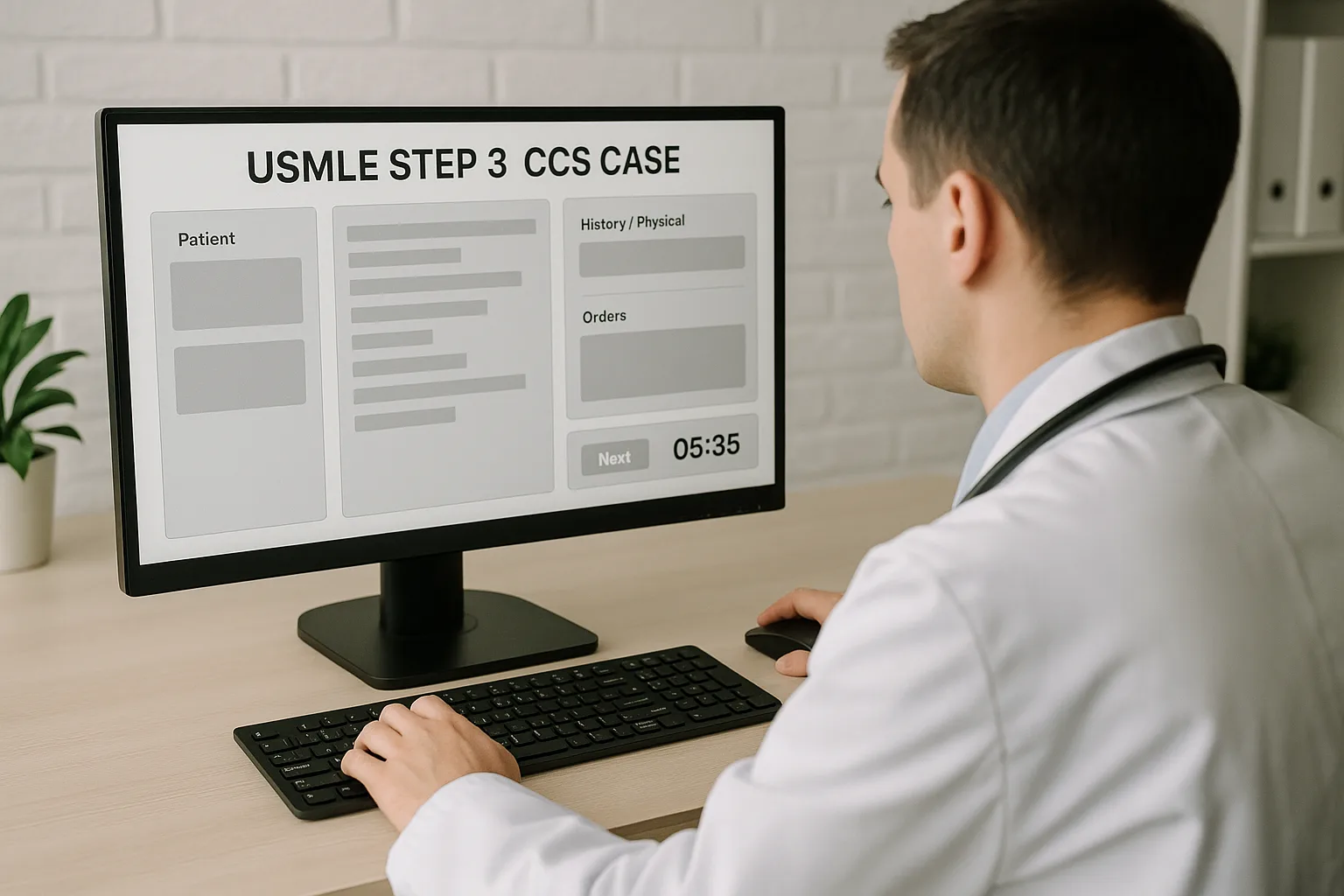
CCS cases are scored for timely, appropriate patient care. You’re credited for lifesaving actions, correct diagnostics at the right moments, and ongoing safety monitoring; you’re penalized for delays and harmful or irrelevant interventions. Cases can be allotted a maximum of 10 or 20 minutes of real time, and the software tracks your clinical trajectory, not your prose. Practically, that means your first minute sets the ceiling for the entire case. If the patient is sick, omissions in the opening minute (e.g., no oxygen, no IV access, no monitoring) may cap your score even if you eventually recover the case. Think of CCS as “manage the room” rather than “solve the riddle.” Start by stabilizing danger signals, then place continuous monitoring and nursing orders that earn background points while you work. Next, make a decisive setting choice (clinic → ED, ED → floor vs ICU) because the wrong venue quietly bleeds points. With stability ensured and the right location chosen, you can order focused tests that will actually change management and advance time to observe a response. When the patient improves, narrow therapy, de-escalate monitoring, and document counseling and follow-up—the exam credits these steady, safe steps. Confirm CCS length and practice environment in the official USMLE materials. How CCS Awards (and Withholds) Points—and Why Speedy Stabilization Wins
The 20-Minute Case Arc
What the Software Cares About
The opening minute is your highest-yield window. Whether the chief complaint is chest pain, shortness of breath, fever, trauma, or altered mental status, the initial move set barely changes: secure the airway and oxygenation, ensure vascular access and monitoring, initiate immediate nursing care, and obtain a minimal set of tests that will guide the next step. You’re building a safety net that both prevents deterioration and accrues background points. Think actions first, then documentation. After the safety bundle, add 2–3 high-impact, diagnosis-directed orders (e.g., aspirin and nitrates for suspected ACS barring contraindications, broad-spectrum antibiotics after cultures for sepsis, bronchodilators and steroids for severe asthma). Don’t drown the case in exhaustive panels—every test should either confirm a working diagnosis or alter management. Finally, immediately decide the appropriate setting (next section) and advance time a few minutes to observe a response; reassess vitals and labs before expanding the work-up. Practice the opening sequence in the official CCS interface to build muscle memory. Your First 60 Seconds: The “First 10 Clicks” Safety Bundle
Action Rationale Common Orders Airway & Oxygen Universal in hypoxemia/resp distress; buys time for diagnostics. O2 via NC/NRB, consider ABG, pulse oximetry continuous. IV Access & Fluids Resuscitation, drug delivery, lactate clearance in sepsis/dehydration. 2 large-bore IVs; isotonic bolus if hypotensive/dehydrated. Monitors Early detection of instability and medication side effects. Cardiac/telemetry, BP q15–30 min, strict I&O, fingerstick glucose. Pain/Temp Control Improves physiology and patient comfort; fever management. Acetaminophen, analgesia as appropriate; avoid masking red flags. Pregnancy Check Guides imaging/medication safety in all reproductive-age patients. Urine/serum hCG prior to radiology or teratogens. Focused Early Tests Fast results that change immediate management. ECG, CXR, CBC, BMP, troponin, lactate, UA, cultures (when indicated).
CCS quietly rewards correct venue selection. In the outpatient setting, unstable physiology (hypotension, hypoxia, altered mental status, active chest pain, severe dehydration) should trigger transfer to the ED immediately. In the ED, disposition hinges on trajectory and needed resources: telemetry, frequent reassessment, and titratable drips generally mean admission. Need for vasopressors, invasive ventilation, or escalating oxygen requirements implies ICU. Conversely, low-risk presentations with normal vitals that respond to minimal interventions often go home with follow-up—and that discharge decision earns points when it’s safe and well documented. Build a few mental switches. If lactate is elevated or MAP is low despite fluids, move to ICU-level care. If ACS is possible (ischemic ECG changes or rising troponin), admit to monitored bed and start guideline-directed therapy. If a patient on supplemental oxygen remains hypoxic and work of breathing is high, escalate to non-invasive ventilation in a monitored setting; failure prompts ICU and airway planning. In OB, heavy bleeding with hypotension means rapid transfer to L&D or OR. In pediatrics, toxic appearance or poor perfusion overrides age-based reassurance—admit and stabilize. Venue decisions are central to the Step 3 blueprint; rehearse them inside the orientation tool and practice cases. Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.Right Patient, Right Place: Clinic, ED, Floor, or ICU?
Admit/ICU Triggers
Safe Discharge Signals
Master your USMLE prep with MDSteps.
100+ new students last month.
After the safety bundle, anchor to a working diagnosis and deploy a compact order set. Keep it problem-based and reversible—start, reassess, narrow. Below are core vignettes you’ll see in multiple disguises and the minimum orders that drive the case forward without clutter. These order sets are intentionally short. Add imaging or consults only if they change the next decision. As you advance time, let results determine your branch: improving vitals → narrow therapy and plan disposition; worsening vitals → intensify support, check for complications, and reconsider the differential. Keep each step purposeful. Problem-Based Order Sets That Move the Needle
Syndrome High-Impact Orders Reassessment Targets Sepsis / Undifferentiated Shock Blood cultures → broad empiric antibiotics; 30 mL/kg isotonic bolus; lactate; early source imaging (CXR/abdominal US/CT as indicated). MAP > 65 mmHg, improving lactate, urine output > 0.5 mL/kg/h; de-escalate ABX with culture data. Chest Pain (ACS) ECG now + repeat; troponins; aspirin; nitrates if not hypotensive/right-sided MI; beta-blocker if stable; statin; cardiology consult. Pain relief, ECG evolution, troponin trend, hemodynamic stability; escalation to cath if STEMI/unstable NSTEMI. Acute Asthma/COPD Exacerbation O2, nebulized bronchodilators, systemic steroids, consider ABG; treat triggers (ABX if COPD + purulence/severe, pneumonia suspected). RR, SpO2, wheeze/work of breathing; avoid over-sedation; consider NIV/ICU if failing. OB: Preeclampsia with Severe Features Magnesium sulfate, IV antihypertensives (labetalol/hydralazine), fetal monitoring, obstetrics consult, consider delivery plan. BP control, neuro status (clonus, headache), reflexes, urine output; maternal/fetal stability. Neonate: Fever/Sepsis Full sepsis work-up, broad empiric antibiotics, fluids, admit to monitored unit; strict I&O; glucose checks. Thermoregulation, perfusion, feeding tolerance, culture results; antibiotic stewardship with narrowing.
One of the most underused CCS levers is monitoring. Continuous pulse oximetry, cardiac telemetry, serial vital signs, strict I&O, neuro checks, and fingerstick glucose (when relevant) add safety and score credit. They also inform the next move. After placing your safety bundle and key diagnostics, advance time deliberately—in short increments early (e.g., 10–30 minutes) to see immediate effects, then in longer increments once the patient stabilizes. Each time jump should be followed by reassessment of vitals, symptoms, and any pending results, with adjustments to therapy. Build a rhythm: (1) stabilize and monitor; (2) order tests/therapy; (3) advance time; (4) check response; (5) escalate or de-escalate. For example, in sepsis after bolus and antibiotics, advance 30 minutes to reassess MAP and lactate trend; if improved, extend the interval, start DVT prophylaxis, and plan step-down. In asthma after bronchodilators and steroids, jump 15 minutes to re-check SpO2 and work of breathing; if stable, move to hourly checks, start discharge planning once ambulation and peak flow improve. Don’t forget therapeutic drug monitoring and safety labs: renal function with nephrotoxic antibiotics, INR if on warfarin, electrolytes with diuresis, glucose with insulin titration. When therapy has achieved goals, place de-escalation orders (wean oxygen, stop IV fluids, narrow antibiotics, transition to PO) and advance time again to confirm stability. This tightening loop—monitor, act, reassess—mirrors real hospital care and aligns with how CCS credits patient-centered management. Familiarize yourself with monitoring options and time controls in the CCS interface via the official practice environment. Monitoring and Time Advancement: Earn Background Points While You Think
The exam rewards diagnostics that change management. Begin with tests that are (1) fast, (2) low-risk, and (3) decisive for your working diagnosis. Avoid shotgun panels that neither clarify the problem nor influence treatment. For chest pain, ECG and serial troponins are non-negotiable; echo or stress testing belongs after stabilization, not before aspirin and nitrates (if appropriate). In suspected PE with low pre-test probability and a negative D-dimer, you don’t need a CT-PA; in high probability with instability, move toward anticoagulation and definitive imaging when safe. A few defaults help: always check pregnancy status in reproductive-age patients before imaging/teratogens; obtain a CXR for respiratory complaints with abnormal vitals or auscultation; order urinalysis when evaluating fever without source; get glucose in altered mental status; order lactate if you suspect sepsis or poor perfusion. When antibiotics are indicated, obtain cultures first when feasible, then treat rapidly—time to therapy matters more than a perfectly curated panel. Resist duplicative testing. If you already have convincing evidence (e.g., classic cholecystitis on US), you don’t need immediate CT unless the course deviates. If an initial test is low yield given the presentation (e.g., head CT for tension-type headache without red flags), skip it. After results return, react: narrow antibiotics, cancel unneeded orders, or pivot the differential. Tie every test to a potential management decision; if you can’t finish the sentence “If positive, I will…; if negative, I will…,” the test probably doesn’t deserve a slot. High-Yield Diagnostics Without Overordering
Many CCS points live in the unglamorous but essential tasks: educating the patient, addressing risk factors, arranging safe follow-up, and documenting return precautions. For smokers, place tobacco cessation counseling and consider NRT. For newly diagnosed diabetes, order nutrition education, glucometer teaching, and a follow-up with primary care or endocrinology. For hospitalized adults, default to VTE prophylaxis unless contraindicated. Confirm vaccination status when relevant (e.g., tetanus after a wound, influenza and pneumococcal in appropriate populations). Discharge requires stability on the lowest safe level of care, tolerating PO if indicated, pain controlled with outpatient-appropriate medications, and clear instructions. Spell out warning signs (“return for fever > 38.3°C, chest pain, syncope, bleeding”) and ensure medications and monitoring are feasible at home. In obstetrics, include fetal kick counts and blood pressure monitoring where relevant; in pediatrics, confirm caregiver comprehension and reliable access. These steps are fast clicks that reliably add points. Place them after stabilization and therapeutic adjustments, then advance time briefly to ensure no late decompensation before ending the case. Counseling, Prevention, and Discharge: The Hidden Points
Discharge & Counseling Quick-List
Train the sequence, not the individual orders. Open the practice software and run “speed drills” in which you execute the safety bundle and venue decision in under 60 seconds, then test your ability to advance time and reassess without forgetting monitoring. Next, rehearse five core syndromes (sepsis, ACS, asthma/COPD, preeclampsia, neonatal fever) until your branch points feel automatic. Keep your differential tight and order only what changes the next move. Verify case counts, timing, and interface controls in the official Step 3 pages and orientation. Then practice until each click path is automatic. Putting It Together: Rehearsal Drills and Rapid-Review Checklist
10-Minute Case Pacing
20-Minute Case Pacing
Rapid-Review Checklist
Sources & Further Practice