Understanding Step 3’s Unique Challenge During Residency
USMLE Step 3 is unlike any prior board exam—it evaluates independent clinical decision-making, longitudinal management, and the ability to synthesize real-time data under fatigue. For residents already stretched thin, the challenge is not intelligence but time logistics and cognitive energy. The question is not if you know the material but whether you can retrieve and apply it under conditions that mirror actual practice. This section outlines the cognitive and structural demands of Step 3 and frames how a six-week plan can integrate naturally into residency life.
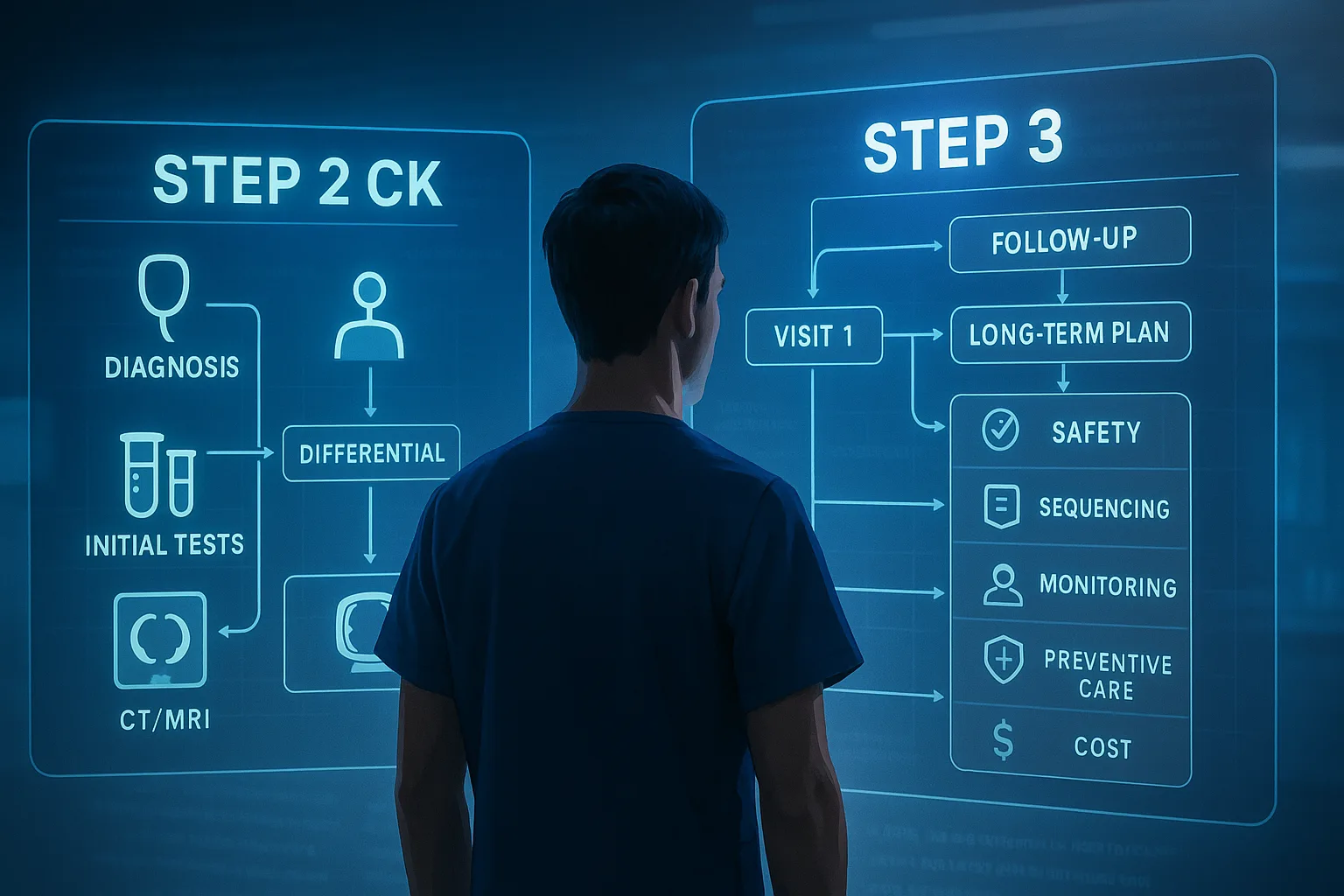
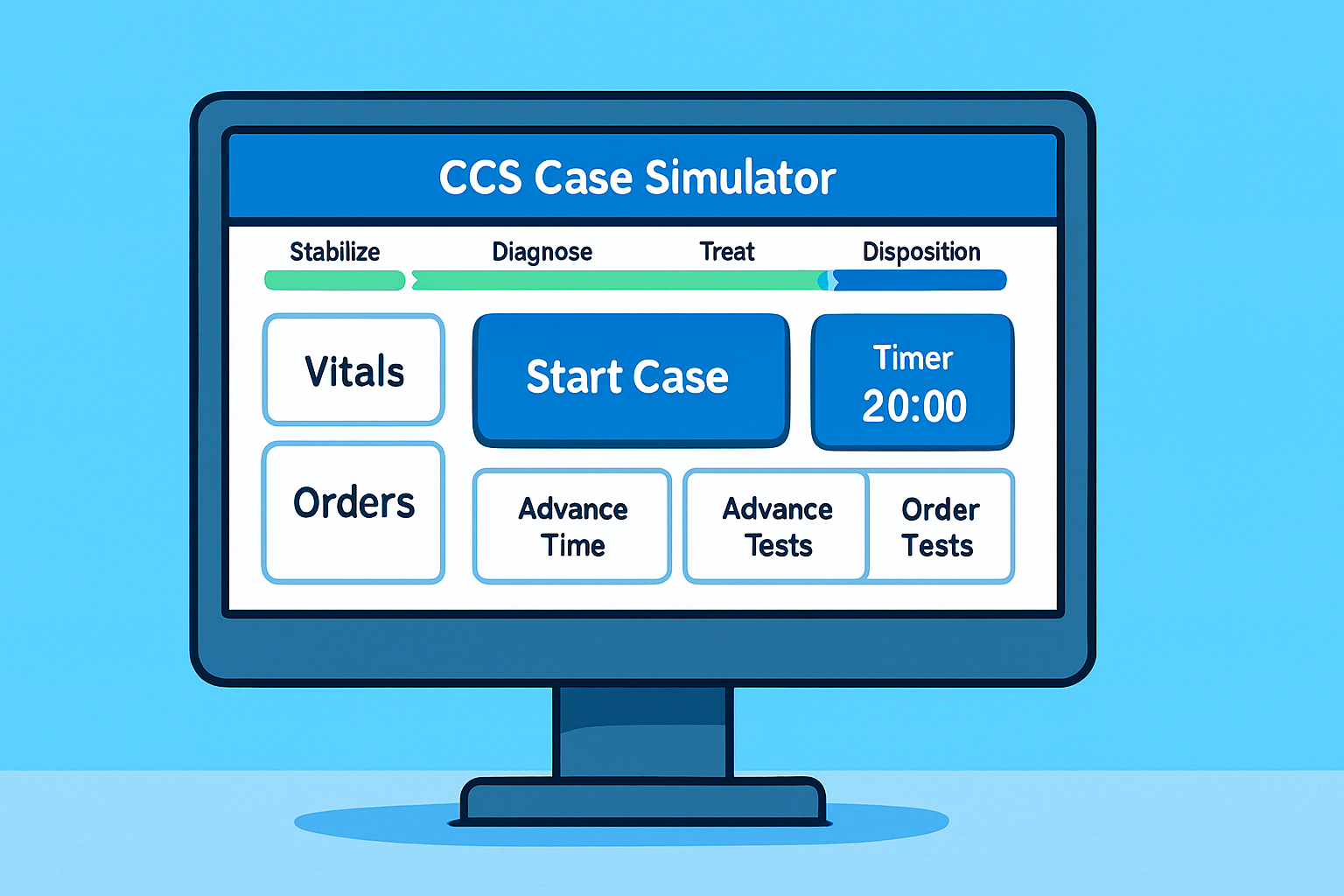
Step 3 contains two full-day testing blocks. Day 1 focuses on multiple-choice Foundations of Independent Practice (FIP), emphasizing biostatistics, ethics, and foundational clinical knowledge. Day 2 centers on Advanced Clinical Medicine (ACM) and the CCS interactive cases. For residents, the shift from passive recall to applied reasoning feels natural—but only if the preparation mimics clinical reasoning speed. The optimal approach is therefore hybrid: short, high-yield question bursts combined with deliberate CCS simulation practice.
MDSteps’ Adaptive QBank streamlines this by sequencing >9000 questions by cognitive load and performance pattern, ensuring each brief study block delivers maximal learning per minute. Integrating QBank analytics into residency downtime lets you target weak systems efficiently.
| Component | Exam Focus | Time Allocation (6 Weeks) |
|---|
| MCQ Practice (FIP/ACM) | Clinical judgment, prioritization | 55% |
| CCS Cases | Diagnostic ordering, management steps | 30% |
| Review & Analytics | Identify persistent weak topics | 10% |
| Exam Simulation | Stamina, pacing | 5% |
This distribution allows residents to reinforce real-world reasoning while maintaining clinical duty balance.
Building a 6-Week Framework Around Residency Rotations
Creating a six-week schedule that respects variable shifts requires adaptive structure rather than fixed hours. The framework below assumes 60-hour clinical weeks with unpredictable calls. The guiding principle: anchor days, not hours. Each day should have one defined academic anchor—morning QBank burst, mid-shift flashcards, or post-call CCS case.
The plan divides into three phases: Foundation (Weeks 1–2), Integration (Weeks 3–4), and Simulation (Weeks 5–6). Within each phase, maintain flexibility but preserve consistency in sequence. MDSteps’ automatic study planner can populate this pattern based on duty hours entered weekly, ensuring you don’t need to micromanage timing.
| Phase | Goal | Primary Tools | Study Blocks/Week |
|---|
| Weeks 1–2 | Solidify core medicine & biostatistics | Adaptive QBank, flashcard reviews | 5 × 1-hr blocks |
| Weeks 3–4 | Integrate CCS cases + reinforce weak areas | CCS Cases Module, analytics dashboard | 6 × 1-hr blocks |
| Weeks 5–6 | Simulate exam days & refine timing | Full-length tests, timed CCS drills | 2 long sessions/week |
Residents often underestimate the benefit of distributed micro-study: a 20-minute flashcard review during sign-out can equate to an hour of tired late-night reading. Scheduling is less about duration than cognitive freshness. Protect one weekly long session—ideally a post-call afternoon—to sustain endurance training for the real exam.
Optimizing QBank Usage for Clinical Integration
Traditional Step 3 prep wastes hours passively reading explanations. Residents need an active retrieval model: answer-analyze-apply. Each QBank block should reinforce not just content but diagnostic sequencing. MDSteps’ Adaptive QBank offers performance analytics by system and competency domain (diagnosis, management, communication), which allows precise reinforcement after clinical shifts. Treat each question as a mini-CCS scenario—document your thought process, then compare to key management steps.
- Block length: 10–15 questions / session (approx. 20 min)
- Review time: 1.5× question time, focus on miss themes
- Tagging: Label each error by reason (cognitive bias, fatigue, knowledge)
- Flashcard conversion: Export misses → automatic deck for Anki review
This deliberate cycle maintains a high retrieval frequency without exceeding the limited daily energy budget. The analytics dashboard helps spot declining accuracy patterns early—an indicator of fatigue or burnout risk rather than content gap.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
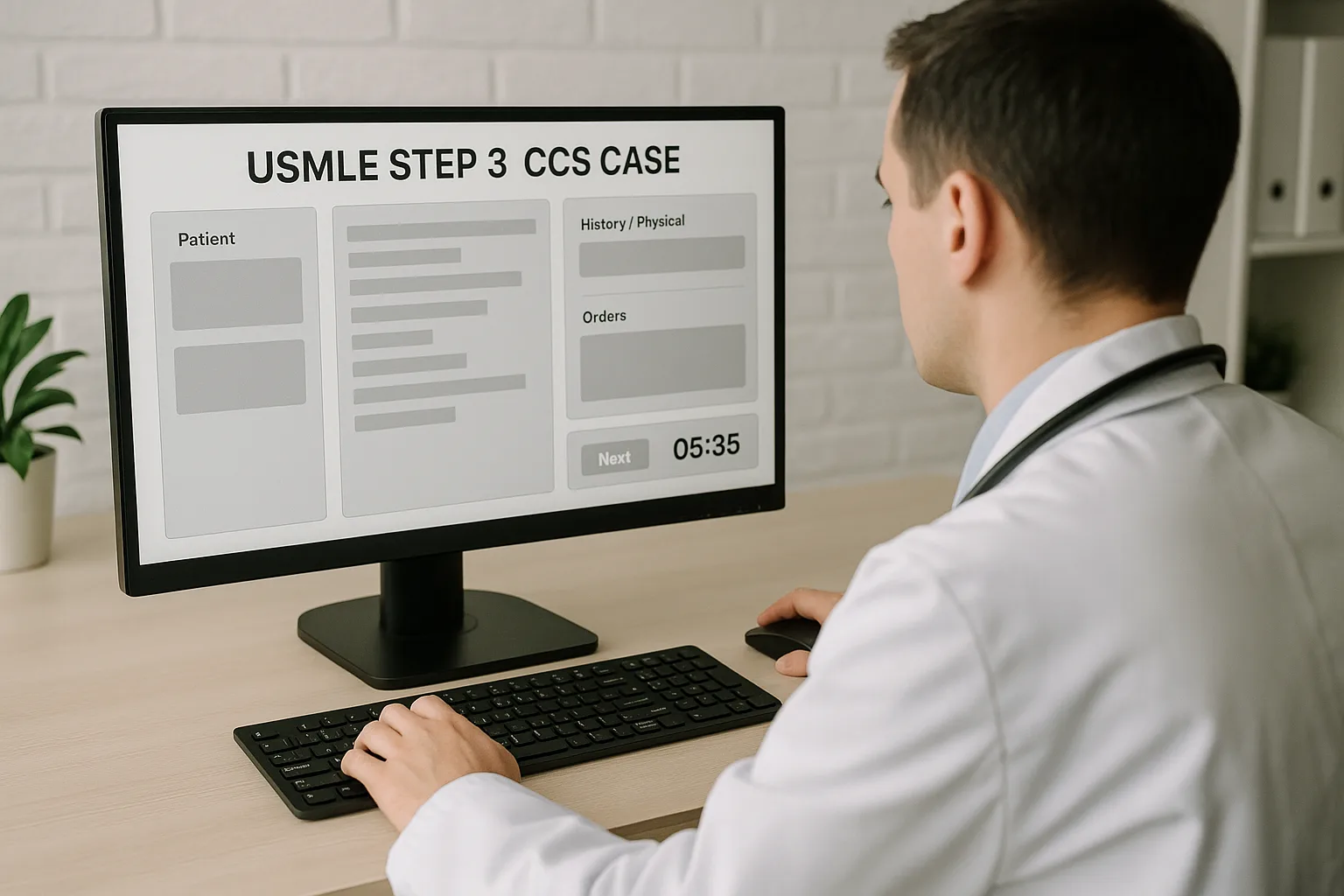
Mastering CCS: From Templates to Real-Time Thinking
The Computer-based Case Simulations (CCS) are the hidden scoring multiplier of Step 3. A resident who performs adequately on MCQs can still significantly boost the overall score by mastering case flow. The CCS platform rewards decisive, guideline-driven action and time control. The following three-tier strategy maximizes performance:
- Template Library (Weeks 1–2): Build default orders for common complaints—chest pain, dyspnea, fever, abdominal pain.
- Timed Drills (Weeks 3–4): Run 10-minute micro-CCS sessions daily using MDSteps’ Live Vitals simulation mode, focusing on appropriate orders and transitions.
- Full Sim (Weeks 5–6): Complete two full CCS practice days replicating exam conditions with the Clock-Advance Decision Tracker checklist.
The goal is automation: knowing what to order without deliberation. Use a clock-advance log to train time sense—when to switch locations, reassess, or end case. During the exam, decisive management yields more points than cautious hesitation.
Time and Energy Management During Heavy Rotations
Residency introduces unavoidable unpredictability—night floats, back-to-back calls, and variable fatigue. Passing Step 3 while working requires precise energy accounting. Use these strategies:
- Energy mapping: Identify your 2–3 highest-alert hours daily and reserve one for active learning.
- Micro-bursts: Replace doom-scrolling breaks with 10-minute flashcard reviews.
- Call-day adaptation: Accept zero study goal on call days; recover next day with light review only.
- Weekend anchor: Dedicate one protected half-day for simulation practice.
Residents who systematize rest paradoxically outperform those who overcommit. Cognitive fatigue directly impairs retrieval accuracy. Integrating MDSteps’ fatigue-aware analytics (tracking performance variability by time of day) can identify when your recall efficiency drops below threshold—an early warning signal to rest before burnout.
Tracking Progress with Analytics and Reflection
Progress in a compressed six-week timeline depends on feedback. MDSteps’ readiness dashboard aggregates question accuracy, CCS case scores, and flashcard retention to generate a live projected score curve. Residents can replicate this logic manually by recording accuracy percentages per week and plotting them against energy levels and sleep quality.
| Metric | Target by Week 6 | Interpretation |
|---|
| Overall QBank Accuracy | ≥ 70 % | Predicts solid FIP performance |
| CCS Completion Rate | ≥ 85 % | Confidence in management automation |
| Flashcard Retention | ≥ 90 % | Effective spacing & recall |
Reflection consolidates metacognition. Every weekend, answer two questions: “Which topic consumed excess time?” and “What pattern did I miss twice?” Writing a 2-minute note enhances transfer to long-term memory and reduces repeat errors.
Exam-Day Strategy and Psychological Readiness
By the final week, most residents possess the knowledge but risk cognitive overload. The goal shifts from acquisition to execution. Here’s how to protect exam-day performance:
- Simulate conditions: Practice one block each morning at exam time.
- Fuel planning: Replicate snacks and hydration used during practice tests.
- Chunk focus: Treat each block as a fresh mini-exam—never carry previous mistakes forward.
- Night-before protocol: Light CCS review only, then sleep 7+ hours.
Confidence stems from controlled repetition. If you’ve followed the six-week framework and maintained ≥ 70 % accuracy on adaptive questions, you’re ready. Trust your data and habit loops more than emotion. Step 3 is as much a test of consistency as knowledge.
Rapid-Review Checklist: 6-Week Step 3 Residency Plan
- Set anchor study blocks 5–6 days/week (20–60 min)
- Target 70 %+ QBank accuracy before week 6
- Integrate CCS micro-drills daily by week 3
- Protect sleep & energy as core study resources
- Use analytics to guide weak-area focus, not emotion
- Simulate two full exam days before test day
- Deploy recovery periods after calls to sustain recall accuracy
- Trust adaptive feedback loops over manual cramming
Completing this realistic six-week plan transforms Step 3 from a logistical burden into a structured performance test that reflects residency-level competence. MDSteps’ adaptive ecosystem—QBank, CCS Cases, flashcards, and analytics—simplifies execution so you can focus on what matters: thinking like an independent clinician.
References & Further Reading:
1. USMLE Step 3 Content Outline & Specifications – usmle.org/step-3
2. Sweller J et al. “Cognitive Load Theory and Instructional Design.” Educational Psychology Review, 2019.
3. Brown P et al. Make It Stick: The Science of Successful Learning. Harvard University Press, 2014.
4. MDSteps Platform – Adaptive QBank and CCS simulation modules.
100+ new students last month.