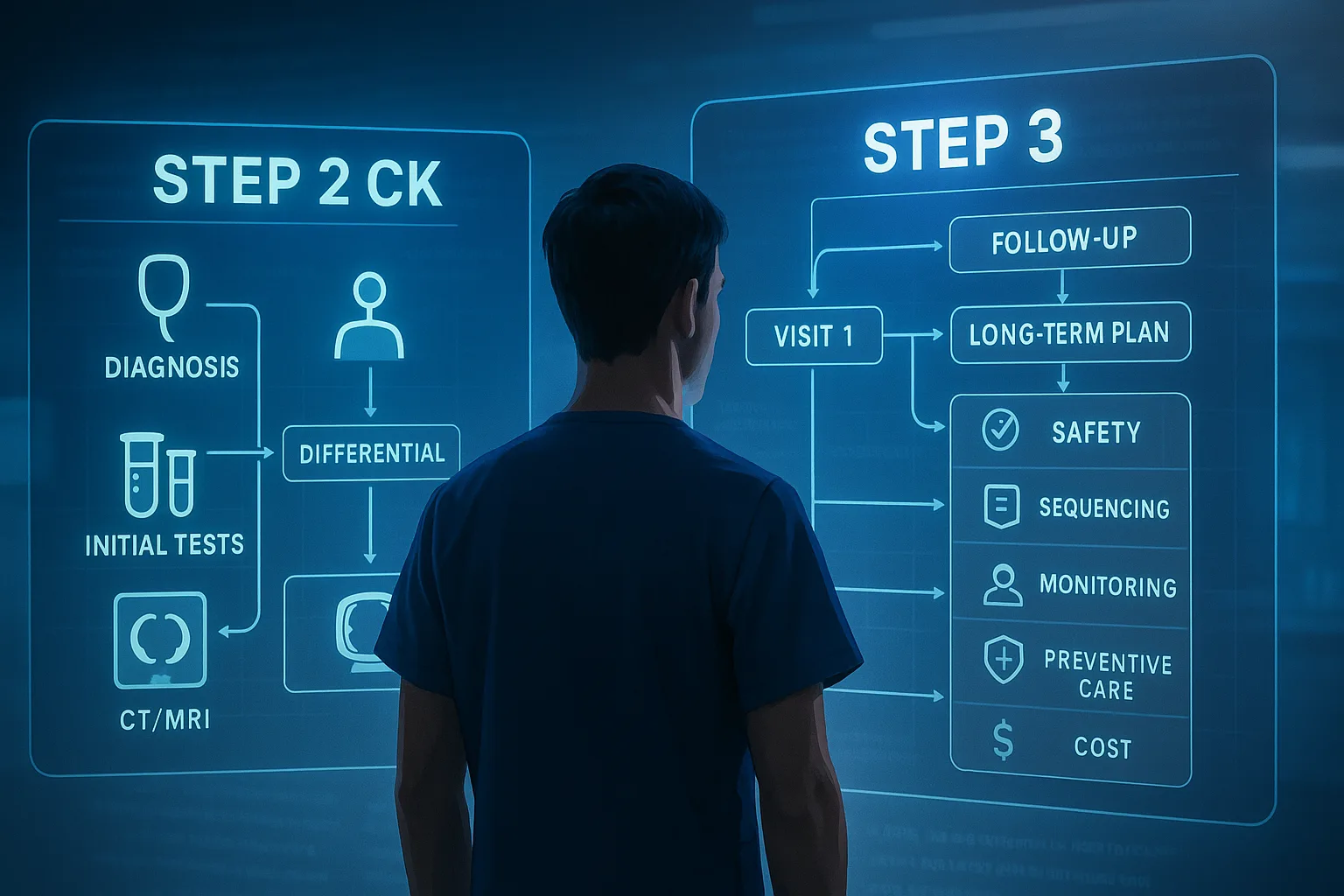
Step 3 is the only USMLE exam built explicitly to test whether you can practice medicine independently. That makes your Step 3 QBank strategy for CCS and MCQ performance fundamentally different from Step 1 or Step 2 CK. Instead of pattern recognition alone, Step 3 evaluates whether you can manage uncertainty, escalate care when necessary, and avoid unsafe choices. A high-yield strategy requires understanding how the exam incorporates patient safety, triage logic, and longitudinal care over multiple days. Within the first 100 words, it is important to highlight that optimizing your Step 3 QBank strategy affects both MCQ accuracy and CCS efficiency, since the exam algorithm looks at time-to-intervention, sequence of orders, and avoidance of contraindicated actions. The core competencies assessed on Step 3 include clinical decision-making, prioritization, and the ability to manage evolving patient scenarios. The MCQs largely mirror Step 2 CK but with broader emphasis on next-step management and outpatient continuity care. The CCS cases, however, evaluate how well you can function in a simulated clinical environment. In these cases, the scoring algorithm rewards not just correct orders, but timely escalation, complete documentation, appropriate counseling, and avoidance of unnecessary or harmful interventions. Test-takers often underestimate how much the CCS component contributes to the final score. Although historically less predictable, recent exam structures have made CCS mastery essential for top performance. When considering how Step 3 evaluates safety, it is crucial to remember that incorrect but benign decisions typically subtract fewer points than unsafe ones. For example, ordering an unnecessary test may reduce efficiency, but omitting oxygen supplementation in a patient with acute respiratory distress can heavily penalize the score. The QBank strategy described in this article emphasizes learning the underlying logic behind high-weighted decisions. You cannot simply memorize checklists; you must internalize a framework that consistently guides safe choices. One of the most effective approaches is to contrast Step 3-style decision-making with the more granular, detail-driven approach typical of earlier USMLE exams. Step 3 emphasizes trajectory over detail. In other words, the exam cares more about directionally correct management sequences rather than memorizing minutiae. This is why targeted practice in a high-quality QBank such as the MDSteps Adaptive QBank is essential. The platform’s adaptive engine exposes you to escalating levels of complexity, forcing you to make decisions with incomplete information—exactly what Step 3 expects. Moreover, because MDSteps automatically generates flashcards based on your missed questions and exports them to Anki, it reinforces your weak areas without additional manual overhead. Another central concept is understanding the integration of inpatient and outpatient care. Step 3 often tests management decisions over time. For example, a patient might present with a relatively benign complaint such as dizziness, but the underlying cause could be arrhythmia, dehydration, or medication toxicity. The exam expects you to perform appropriate initial diagnostics and then continue monitoring, adjusting therapy based on new data. CCS cases simulate this by requiring follow-up intervals, repeating vitals, and checking on labs. Using MDSteps Live Vitals CCS cases prepares you for these longitudinal decisions because the simulation shows dynamic physiological changes rather than static snapshots. To maximize performance, you must also maintain awareness of Step 3’s unique scoring model. Unlike Step 1 and Step 2 CK, which rely strictly on MCQs, Step 3 assigns substantial weight to CCS. A strong MCQ performance can be dragged down by poor CCS sequencing. Conversely, excellent CCS performance can buffer a middling MCQ score. This makes it essential to integrate CCS practice into your regular QBank schedule rather than saving it for the end. Daily, low-volume exposure reinforces clinical flow and builds the intuition needed for real-time decision-making. Below is a quick-hit summary of Step 3’s emphasis areas: Understanding this competency map helps you allocate your time intelligently. The remainder of this article will build a systematic strategy for integrating QBank practice, CCS workflows, and exam-day decision logic to maximize your Step 3 performance. Understanding How Step 3 Evaluates Clinical Judgment
Domain MCQs CCS Cases Clinical Safety High Very High Next-Step Logic High High Time-Based Decisions Moderate Very High Broad Differential High Moderate Communication & Counseling Moderate High
Creating an intentional Step 3 QBank schedule is a major component of any effective Step 3 QBank strategy for CCS and MCQ performance. Unlike the preclinical exams, Step 3 rewards consistent, moderate-volume practice over cramming. Most examinees are residents or international medical graduates already working full-time or managing variable schedules. Therefore, you must design a plan that is both sustainable and aligned with how the exam distributes content. A productive Step 3 schedule aligns with four principles: steady exposure, spiraled review, CCS integration, and periodic long-block stamina training. Steady exposure means practicing questions nearly every day, even if you are only completing a single block. Spiraled review involves returning to previously tested concepts in varied contexts. Integrating CCS early prevents cognitive overload later. And stamina training ensures that your brain can function effectively over two days of testing. Most high-performing examinees use a two-phase study model. Phase 1 emphasizes building a knowledge and decision-making foundation through MCQs and targeted reading. Phase 2 focuses on exam simulation, CCS timing, and refining decision speed. A three- to six-week timeline works well for most learners. Those with heavier clinical rotations may need eight to twelve weeks with lower daily question volumes. The MDSteps Adaptive QBank makes schedule planning easier by generating automatic daily study plans based on your performance metrics. Instead of choosing topics manually, the platform continuously analyzes weak areas and rotates them back into your sessions. This reduces time wasted on choices and streamlines your cognitive load. The analytics dashboard also shows readiness projections, topic mastery heatmaps, and performance percentiles, making it easier to know when to shift from Phase 1 to Phase 2. Below is a sample three-week schedule for a resident with limited daily availability: This structure helps maintain momentum while gradually increasing cognitive demand. It also prevents burnout, particularly important for trainees working irregular hours. Adding weekly review sessions to revisit missed questions helps solidify learning. Since MDSteps automatically generates flashcards from missed items, you can review these decks during commutes, breaks, or downtime between patients. Another important consideration is choosing the appropriate mode for MCQ practice. Always use timed mode. Untimed mode eliminates the time pressure integral to real-life clinical decision-making. Step 3 MCQs assess whether you can make decisions when time is limited, especially when facing multi-step reasoning problems or management sequencing questions. Timed blocks also train your brain to function under exam pacing. As part of your schedule, set aside specific blocks for cumulative review. At least once a week, complete a mixed block rather than a system-based block. Mixed blocks help you mimic Step 3’s distribution and develop the flexibility needed for rapid context-switching. This prevents fatigue-related errors on exam day and exposes you to a more realistic variety of presentations. Finally, your schedule must include built-in recovery. Most examinees underestimate the cognitive burden of work plus studying. One day each week should be light review only. This active recovery helps sustain long-term performance and prevents burnout. Since Step 3 spans two test days, entering the exam rested is essential. Designing a High-Yield Step 3 QBank Schedule
Week Daily MCQs Weekly CCS Cases Goal 1 15–20 timed 3 cases Identify weak systems and management gaps 2 20–25 timed 5–6 cases Build pattern recognition; improve CCS flow 3 30 timed 8–10 cases Exam simulation; refine safety and efficiency
For Step 3, one of the most efficient ways to enhance MCQ scores is through targeted pattern recognition. The exam rewards the ability to rapidly identify the core of a clinical vignette and eliminate distractors. More importantly, it emphasizes management logic. A strong Step 3 QBank strategy for CCS and MCQ performance incorporates daily exposure to timed MCQs to refine your pattern recognition and decision sequencing skills. Effective Step 3 pattern recognition hinges on several principles: identifying red flags, prioritizing patient stability, applying next-best-step logic, and avoiding unsafe decisions. Many examinees mistakenly focus on memorizing isolated facts rather than understanding the dynamic reasoning process behind correct answers. To achieve consistently strong performance, you must internalize a mental framework for triage, diagnostics, and management. The first key element is learning to identify red-flag features within the vignette. These elements—such as hypotension, mental status changes, new focal neurologic deficits, severe infections, or signs of organ failure—shift the management pathway toward stabilization and emergent intervention. Recognizing these signals allows you to prioritize airway, breathing, circulation, or rapid imaging when appropriate. Overlooking subtle signs of deterioration is one of the most common pitfalls among examinees. Next, refine your next-best-step reasoning. This skill is especially important for Step 3 because the exam prioritizes practical decision-making. Questions often present several medically reasonable options, but only one represents the safest, most efficient next action. You must learn to resist the temptation to “do everything” and instead choose the intervention that immediately addresses the highest-risk problem. Practicing this repeatedly in timed MCQ blocks helps reinforce the prioritization logic ingrained in high-level clinical practice. Another important concept is learning how Step 3 weighs the risks of unnecessary testing. In many outpatient scenarios, the correct answer is reassurance or lifestyle modification, not laboratory or imaging studies. The exam penalizes overuse of resources. This is why MDSteps Adaptive QBank deliberately includes cases where the correct answer is “no intervention,” helping train the restraint necessary for safe clinical practice. To strengthen your recognition skills, you must structure MCQ review sessions effectively. Instead of reading every explanation in full, focus on three questions after each block: (1) Why was the correct answer best? (2) Which distractor was most tempting? (3) Why was that distractor wrong? This approach sharpens your ability to distinguish between plausible but incorrect options. MDSteps’ explanation format supports this by including “most commonly chosen distractor analysis,” which helps target your cognitive traps. Another high-yield method is constructing concise summary notes for repeated management principles. For example, you might create short lists for chest pain workup, management of sepsis, initial evaluation of syncope, or pediatric fever algorithms. Summaries help consolidate key steps without forcing you to memorize full explanations. This approach is useful in residency, where time is limited. Timed blocks also help strengthen endurance. Because Step 3 spans two exam days, you must develop the cognitive stamina to maintain focus over multiple hours. Gradually increasing your block volume mimics exam-day pacing and reduces fatigue-related errors. If you frequently experience time pressure, practice eliminating obviously incorrect options quickly. This reduces cognitive load and preserves mental resources for more complex questions. Lastly, leverage MDSteps analytics to refine your pattern recognition. The platform tracks your performance across topic clusters and identifies recurrent error patterns. For example, if you repeatedly miss endocrine management questions or misinterpret laboratory patterns in hematology, the system automatically schedules targeted review sessions and generates flashcards for repeated practice. By implementing these strategies, your MCQ performance improves steadily. Pattern recognition accelerates with practice, enabling you to navigate complex Step 3 questions with confidence. Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.Optimizing MCQ Blocks with Targeted Pattern Recognition
Master your USMLE prep with MDSteps.
100+ new students last month.
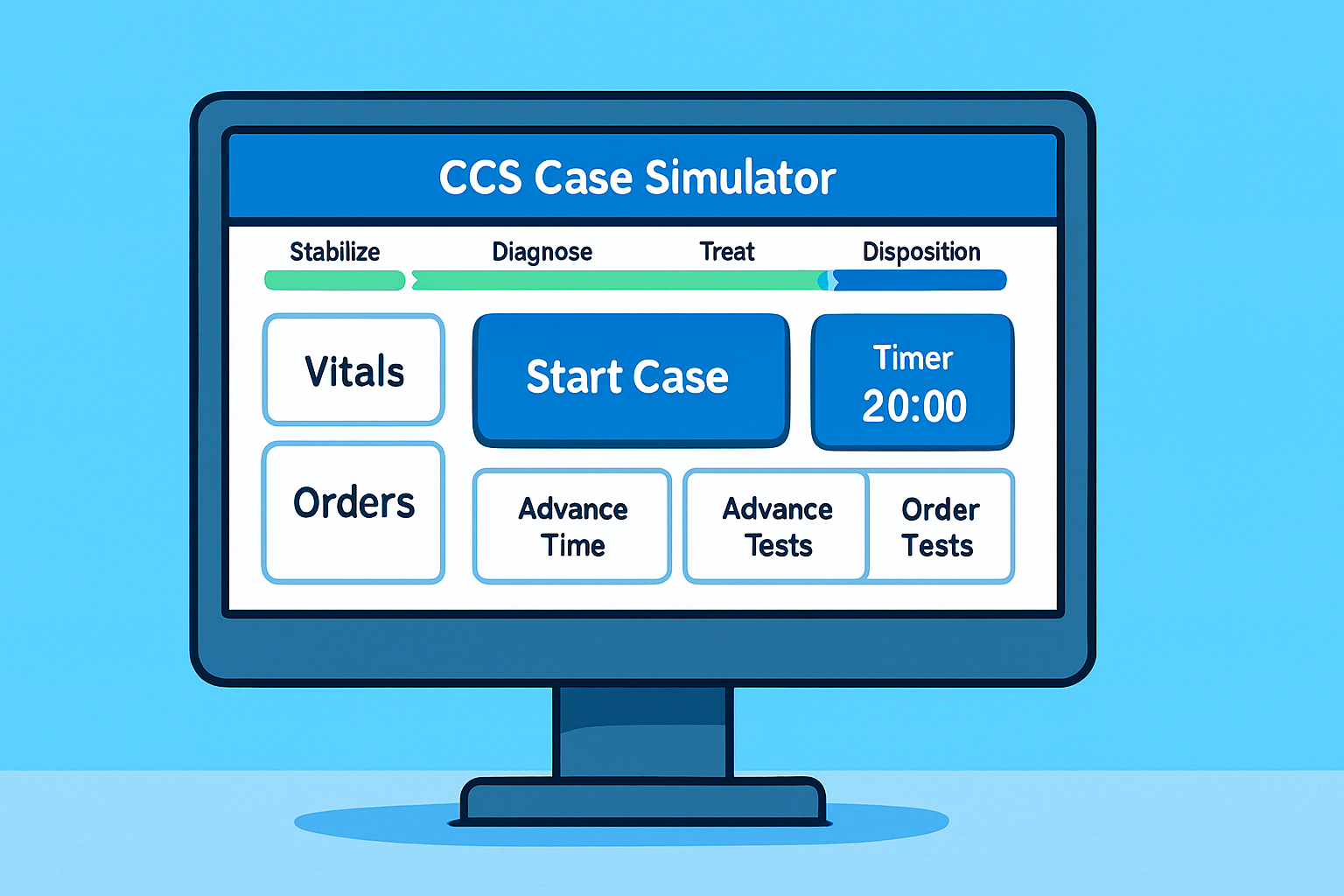
The CCS portion of Step 3 represents a unique challenge for examinees because it tests not only clinical reasoning but also procedural fluency. A robust Step 3 QBank strategy for CCS and MCQ performance requires early and consistent CCS practice. Unlike MCQs, CCS cases evaluate your ability to manage a patient longitudinally, respond to dynamic changes, and escalate care appropriately. The exam software simulates real-time physiology. Learning to navigate this environment efficiently requires structured practice. The first principle of CCS success is workflow automation. You must internalize a standardized case-opening routine that you execute automatically. This reduces cognitive load and minimizes errors. A reliable routine includes confirming patient stability, initiating vitals and monitoring, ordering essential baseline studies, and considering immediate interventions based on presenting complaints. By creating a habitual sequence, you avoid forgetting critical early steps. For example, nearly every acute CCS scenario benefits from early placement of pulse oximetry, blood pressure monitoring, and cardiac monitoring, combined with a thorough physical examination. Many examinees lose points because they delay or omit these essential interventions. Similarly, most cases require basic laboratory testing such as CBC, CMP, urinalysis, ECG, and chest X-ray. By automating these orders, you ensure that evaluations proceed efficiently. MDSteps Live Vitals CCS cases emphasize these fundamentals by simulating realistic physiological changes that respond to your interventions. The second principle is timely escalation. CCS cases reward early transfer to higher levels of care when clinically indicated. If a patient demonstrates hemodynamic instability, severe hypoxia, or signs of organ failure, immediately escalate to ICU-level monitoring. Delayed escalation is heavily penalized. Practicing cases that present vague symptoms helps train your escalation reflexes. The third principle is longitudinal follow-up. Many examinees forget to advance the clock appropriately or re-check vital signs and laboratory values. CCS cases include hidden time-sensitive scoring events. If you do not re-evaluate the patient at appropriate intervals, you miss opportunities to intervene. Scheduling follow-up in the case interface reinforces this habit. Efficient CCS performance also requires understanding when not to over-order. Unnecessary tests reduce your score. By focusing on essential clinical pathways, you maintain high-value care. MDSteps cases help internalize cost-effective practice by guiding you toward evidence-based sequences. Finally, end-of-case wrap-up often determines score differentials. Always re-examine the patient, provide counseling, adjust medications, and schedule follow-up appointments. These details elevate your performance from adequate to exceptional. Building CCS Mastery Through Workflow Automation
Most examinees make the mistake of postponing CCS practice until the final week before the exam. This approach is ineffective because CCS success relies on building fluency, not cramming information. A strong Step 3 QBank strategy for CCS and MCQ performance integrates CCS into your daily study schedule. Even a few cases each week builds long-term proficiency. Start with low-stress cases to familiarize yourself with the interface, then transition to more complex scenarios. MDSteps Live Vitals CCS cases offer dynamic simulations that train realistic decision-making. Practice acute settings early to develop rapid response reflexes. Reserve outpatient continuity cases for later, when you have mastered basic workflow automation. Integrating CCS into your routine also benefits your MCQ performance. CCS scenarios reinforce management sequences that appear in MCQs. By repeatedly practicing clinical pathways, you internalize decision-making frameworks that transfer directly to timed questions. Daily CCS exposure also sharpens your clinical intuition. Make CCS a consistent habit. Even brief practice yields compounding returns. Integrating CCS Practice into Your Daily Routine
One of the strongest predictors of Step 3 score improvement is the ability to identify and correct weak areas efficiently. A sophisticated Step 3 QBank strategy for CCS and MCQ performance relies on continuous data feedback. MDSteps provides an advanced analytics dashboard that tracks mastery, identifies knowledge gaps, and recommends targeted review sessions. Using these analytics, you can quickly identify recurring patterns in your errors. For example, if you frequently miss questions on antibiotic selection or stroke management, the system automatically schedules these topics for review. It also generates flashcards based on your misses, creating a personalized study deck that reinforces weak areas. Analytics also reveal your pacing issues. If you consistently run out of time during MCQ blocks, the platform highlights this trend and recommends pacing drills. By tracking your progress over time, you know exactly when you are ready to transition from learning mode to exam simulation mode. This data-driven approach streamlines preparation and maximizes efficiency, especially for busy residents. Instead of guessing where to spend your time, you follow the insights derived from your performance patterns. Data-Driven Refinement Using MDSteps Analytics
Step 3 is unique because it spans two days, each testing different cognitive domains. A successful Step 3 QBank strategy for CCS and MCQ performance prepares you for the logistical and mental demands of the exam. Day 1 focuses heavily on foundational science and general medicine, while Day 2 emphasizes advanced clinical management and CCS cases. Stamina, pacing, and mental resilience play critical roles. Plan your breaks strategically. Hydrate adequately but avoid excessive caffeine. Eat predictable foods that will not cause energy crashes or gastrointestinal discomfort. Wear comfortable clothing. Bring approved snacks. Review your CCS workflow the night before Day 2, but avoid heavy studying. A brief warm-up is enough to keep your mind sharp without fatiguing yourself. On the morning of the exam, visualize your opening case routine. This mental rehearsal boosts confidence and improves performance. During the exam, remain flexible. If a case or MCQ seems unusually difficult, maintain composure. Your score is based on aggregate performance. Do not let one challenging item derail your confidence. Keep your focus forward. Two-Day Exam Logistics and Mental Performance
By combining intentional MCQ practice, structured CCS workflows, and data-driven refinement, you create a high-yield Step 3 preparation system. Consistency, efficiency, and clinical judgment form the core of your performance. With deliberate practice and a strategic approach, you can enter the exam confident and prepared. Rapid-Review Checklist & Final Prep Plan