1) Orientation & Exam Strategy: Reading the Stem Through the Receptors
Autonomic pharmacology on Step 1 is ultimately a pattern-recognition game grounded in receptor biology. Vignettes usually reveal the answer through a triad: (1) a drug’s dominant receptor profile (α1, α2, β1, β2, β3, M1–M3, Nn, Nm), (2) the immediate physiologic effect (e.g., ↑ systemic vascular resistance, bronchodilation, AV nodal slowing), and (3) the baroreflex-mediated response (reflex tachycardia or bradycardia). Your task is to sort those clues quickly and map them to prototypic agents. The most reliable entry point is to identify the primary effector variable in the stem—mean arterial pressure (MAP), heart rate (HR), or airway caliber—and then ask which receptor pathway most cleanly explains the change.
For vasoactive questions, anchor on MAP and pulse pressure. Pure α1 agonists (e.g., phenylephrine) cause arteriolar vasoconstriction → ↑ MAP and ↑ pulse pressure with reflex bradycardia. Pure β1/β2 agonists (e.g., isoproterenol) reduce peripheral resistance via β2 while increasing inotropy via β1 → ↓ MAP, ↑ pulse pressure, and reflex tachycardia. Norepinephrine, dominated by α1 with β1 support and minimal β2, raises MAP strongly; heart rate may fall from baroreflex despite intrinsic β1 stimulation. Epinephrine behaves in a dose-dependent manner (β2/β1 at low dose; α1 dominates at higher dose); the vignette’s context (e.g., anaphylaxis vs local hemostasis) tells you where on that curve the patient sits.
Cholinergic stems hinge on which receptor family is targeted. Muscarinic agonism produces DUMBBELSS (Diarrhea, Urination, Miosis, Bronchospasm/bronchorrhea, Bradycardia, Emesis, Lacrimation, Sweating, Salivation). Nicotinic receptor effects split between autonomic ganglia (Nn) and neuromuscular junction (Nm); organophosphate poisoning often starts with muscarinic excess but adds weakness/fasciculations via Nm. Antimuscarinics invert the muscarinic picture (mydriasis, tachycardia, anhidrosis, urinary retention, ileus, hyperthermia due to impaired sweating).
Exam moves: (1) Write a tiny “receptor compass” in the margin (Gq: α1/M1/M3 → ↑Ca²⁺; Gi: α2/M2 → ↓cAMP; Gs: β1/β2/β3 → ↑cAMP). (2) For any drug, name two prototype tissues where that receptor “speaks loudly,” then predict benefits and adverse effects from those tissues. (3) When a blood pressure change is present, ask whether the HR change is reflex or direct. (4) Use contraindication logic to eliminate distractors (e.g., nonselective β-blocker worsening bronchospasm in asthma; α1 blocker precipitating orthostatic hypotension in the elderly or when combined with PDE5 inhibitors). This disciplined approach converts dense stems into a short mechanistic path to the answer.
2) Core Receptor Physiology: Transducers, Tissues, and First-Order Predictions
Autonomic receptors are information translators. Their G-protein coupling determines the intracellular second messenger and thereby the organ-level phenotype. Gq (α1, M1, M3) → phospholipase C activation → IP3/DAG → ↑ intracellular Ca²⁺ and smooth muscle contraction or glandular secretion. Gi (α2, M2) → ↓ adenylyl cyclase → ↓ cAMP, often dampening neurotransmitter release (α2) or slowing nodal pacemaking (M2). Gs (β1/β2/β3) → ↑ cAMP; in the heart, cAMP–PKA phosphorylation boosts inotropy and chronotropy; in smooth muscle (e.g., bronchioles), cAMP relaxes myosin light-chain kinase, causing relaxation.
Tissue “loudness” for receptors sets predictable outcomes. α1 is strongest in arteriolar/venous smooth muscle (vasoconstriction), pupillary dilator (mydriasis without cycloplegia), and bladder trigone/sphincter (urinary retention). α2 lives on presynaptic terminals (↓ NE release) and pancreatic β-cells (↓ insulin). β1 dominates in SA/AV node and ventricular myocardium (↑ rate and force) and juxtaglomerular cells (↑ renin). β2 is prominent in vascular beds of skeletal muscle and bronchioles (vaso/bronchodilation) and in the uterus (relaxation). β3 promotes lipolysis and detrusor relaxation. M1 (CNS, enteric) modulates cognition and gastric acid; M2 slows the heart; M3 contracts smooth muscle (bronchoconstriction, detrusor contraction) and glands (sweat, tears, saliva) and causes pupillary constriction with accommodation (sphincter pupillae + ciliary muscle).
| Receptor | G-protein | Dominant Tissues | Key Physiologic Effects | Prototype Agonist | Prototype Antagonist |
| α1 | Gq | Arterioles, venules, iris dilator, bladder sphincter | Vasoconstriction, mydriasis, urinary retention | Phenylephrine | Prazosin (α1-selective) |
| α2 | Gi | Presynaptic terminals, CNS, pancreatic β-cells | ↓ NE release, sedation/analgesia, ↓ insulin | Clonidine | Yohimbine |
| β1 | Gs | Heart, JG cells | ↑ HR/contractility, ↑ renin | Dobutamine | Metoprolol (β1-selective) |
| β2 | Gs | Bronchioles, skeletal muscle vasculature, uterus | Bronchodilation, vasodilation, tocolysis | Albuterol | Propranolol (nonselective) |
| β3 | Gs | Adipocytes, bladder detrusor | Lipolysis, detrusor relaxation | Mirabegron | — |
| M1 | Gq | CNS, enteric nervous system | Cognition, gastric acid secretion | Pilocarpine | Atropine (nonselective) |
| M2 | Gi | SA/AV node | ↓ HR, ↓ conduction | Bethanechol (nonselective M agonist) | Atropine |
| M3 | Gq | Bronchi, GI, bladder, glands, eye | Bronchoconstriction, peristalsis, urination, secretion, miosis/accommodation | Carbachol | Atropine, Ipratropium (M3-targeted in airways) |
| Nn | Na⁺/K⁺ channel | Autonomic ganglia, adrenal medulla | Fast depolarization of postganglionic neurons | Nicotine | Hexamethonium (historical) |
| Nm | Na⁺/K⁺ channel | Neuromuscular junction | End-plate depolarization → contraction | Succinylcholine (depolarizing) | Rocuronium (non-depolarizing) |
Keep this matrix in mind: coupling predicts intracellular signal; tissue distribution predicts organ response; prototypes embody the testable extremes. When a stem alters any link in this chain (e.g., “patient on a nonselective β-blocker inhales albuterol but bronchospasm persists”), the correct inference is nearly automatic.
3) Adrenergic Agonists: Pressors, Inotropes, and Dose-Dependent Epinephrine
Phenylephrine is the archetypal pure α1 agonist: it elevates SVR, raises MAP, widens pulse pressure, and evokes reflex bradycardia. Uses include nasal decongestion (vasoconstriction), mydriasis without cycloplegia, and short-term hypotension management. Norepinephrine (α1 > β1 ≫ β2) is a first-line vasopressor in distributive shock (sepsis): dominant α1 raises MAP; β1 improves cardiac performance; small β2 effect means limited vasodilation. HR often falls or remains unchanged due to baroreflex overwhelming β1 chronotropy. Epinephrine is dose-dependent: at low dose (β2/β1), it reduces SVR modestly and increases HR/CO; at high dose, α1 dominates, raising SVR/MAP. In anaphylaxis, epinephrine’s β2 bronchodilation and mast-cell stabilization plus α1 vasoconstriction are lifesaving; IM route avoids arrhythmogenic peaks.
Isoproterenol (β1 = β2) decreases SVR (β2) while increasing HR/inotropy (β1), yielding reduced MAP and pronounced reflex tachycardia. It is not a routine pressor; it is instead a teaching tool for β physiology and occasionally used for torsades from bradyarrhythmias. Dobutamine (β1 > β2, α1) increases inotropy and, to a lesser extent, chronotropy; the net vascular effect depends on preparation/isoforms but typically mild vasodilation (β2) offsets weak α1. Use short-term in cardiogenic shock when raising CO is the goal.
Selective β2 agonists (albuterol, salmeterol, formoterol) relax bronchial smooth muscle via cAMP and are cornerstones in asthma/COPD. Systemic β2 agonists can cause tremor, hypokalemia (intracellular K⁺ shift), and tachycardia (direct β1 spillover at high doses and reflex from β2 vasodilation). Mirabegron (β3 agonist) relaxes detrusor to treat overactive bladder; watch for hypertension from incidental β1/β2 activity at higher exposures.
| Agent | Dominant Profile | MAP | Pulse Pressure | Reflex HR | Signature Clinical Uses |
| Phenylephrine | α1 | ↑↑ | ↑ | ↓ (brady) | Vasoconstrictor, mydriasis, decongestant |
| Norepinephrine | α1 > β1 | ↑↑ | ↑ | ↔/↓ | Septic/distributive shock |
| Epinephrine (low) | β2/β1 | ↘ | ↑ | ↑ (tachy) | Anaphylaxis (overall IM dosing spans β + α benefits) |
| Epinephrine (high) | α1/β1 | ↑ | ↑ | ↔/↓ | Hemostasis, severe hypotension |
| Isoproterenol | β1 = β2 | ↓ | ↑ | ↑↑ | Beta-physiology demonstrations; rare bradyarrhythmia uses |
| Dobutamine | β1 (±β2, α1) | ↔/↓ | ↑ | ↑ | Cardiogenic shock, stress testing |
Two high-yield caveats: (1) Local tissue receptors may dominate over “whole-body” predictions (e.g., epinephrine via α1 vasoconstriction reduces diffusion from a local anesthetic injection site). (2) β2-mediated K⁺ shifts can precipitate or mask hypokalemia and provoke arrhythmias, especially with digoxin or diuretics—watch electrolytes in stems featuring high-dose inhaled β agonists or nebulized continuous therapy in the ED.
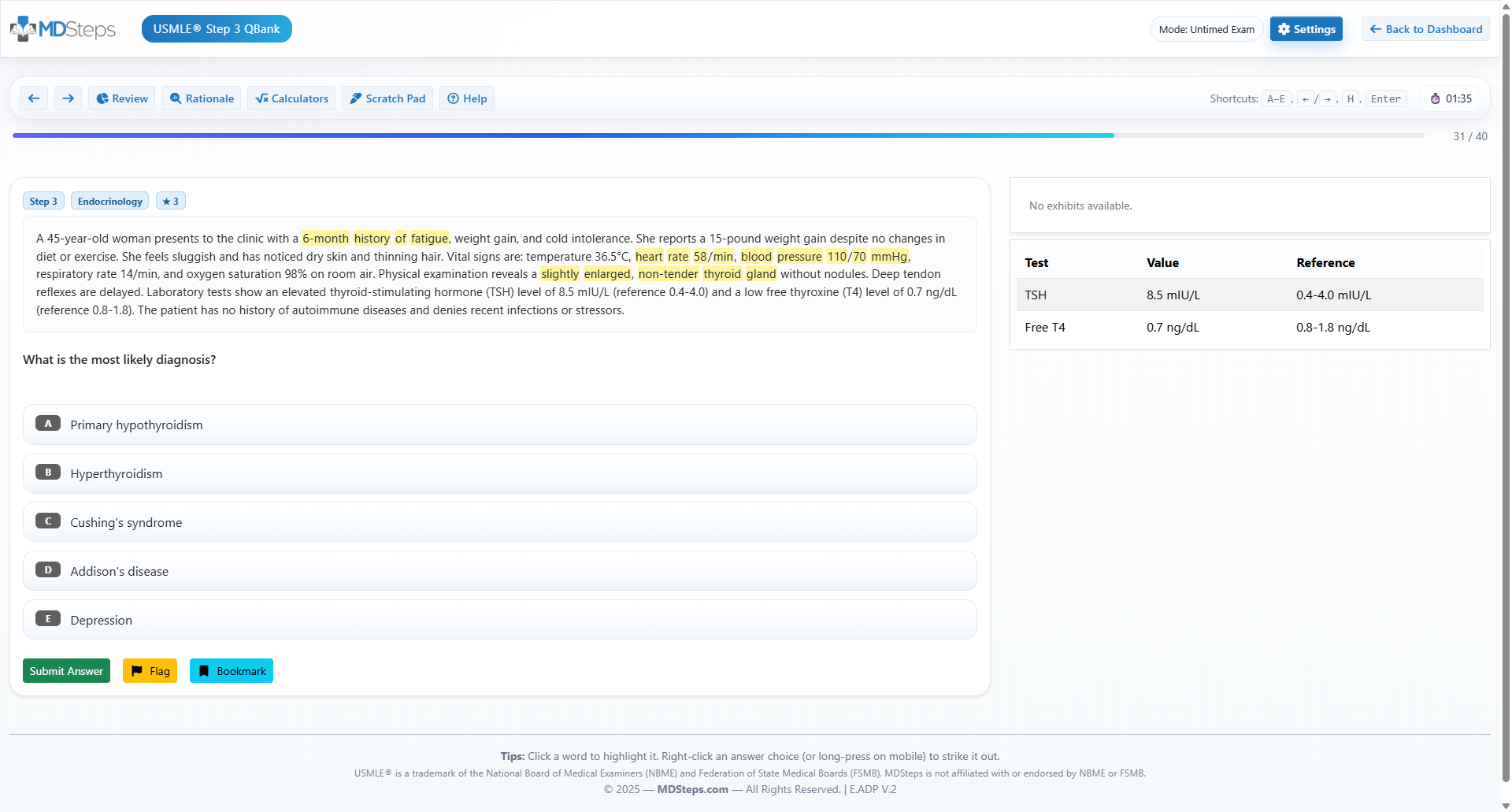
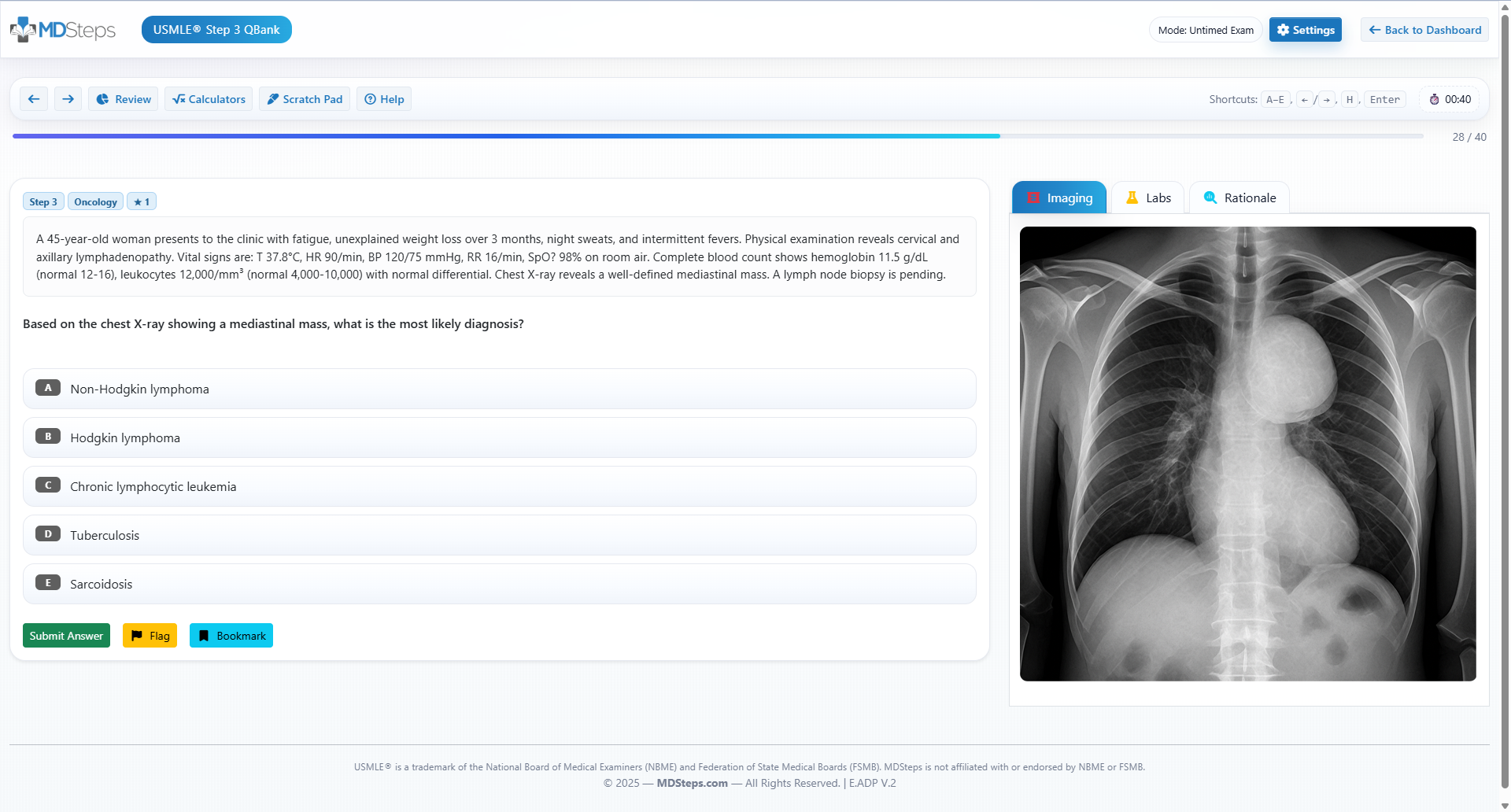
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
4) Adrenergic Antagonists & Mixed Agents: Therapeutic Levers and Reflex Logic
α blockers. Noncompetitive, irreversible phenoxybenzamine is classic for preoperative control in pheochromocytoma; competitive phentolamine reverses catecholamine-mediated vasoconstriction or extravasation and treats MAOI/tyramine crises. Selective α1 antagonists (prazosin, terazosin, doxazosin) reduce SVR and relieve bladder outlet obstruction in BPH by relaxing smooth muscle at the bladder neck and prostate; first-dose orthostatic hypotension and reflex tachycardia are common. Tamsulosin is more α1A-selective (uroselective), mitigating BP effects but not eliminating dizziness.
β blockers. Cardioselective β1 antagonists (metoprolol, atenolol, esmolol) slow HR/AV conduction and reduce myocardial oxygen demand; they are better tolerated in reactive airway disease than nonselective agents but are not fully risk-free. Nonselective β blockers (propranolol, nadolol) also block β2, leading to bronchospasm and masking of hypoglycemia; they lower portal pressures (variceal prophylaxis) and control hyperthyroid sympathetic symptoms. Mixed α1/β blockers (labetalol, carvedilol) reduce afterload without as much reflex tachycardia—useful in aortic dissection (labetalol) and systolic heart failure (carvedilol improves survival via neurohormonal dampening).
Reflex and special cases. Blocking β2 removes vasodilatory buffering and can unmask α-mediated vasoconstriction (e.g., epinephrine in a patient on propranolol → severe hypertension). β blockers blunt glucagon-mediated hepatic glucose output and mask adrenergic signs of hypoglycemia; sweat/cholinergic signs persist. Agents with intrinsic sympathomimetic activity (ISA) like pindolol cause less resting bradycardia but are avoided post-MI. Some β blockers have membrane-stabilizing (“quinidine-like”) effects at high doses.
| Class | Examples | Key Clinical Effects | High-Yield Uses | Pitfalls |
| Irreversible α | Phenoxybenzamine | Long α blockade | Pheochromocytoma pre-op | Reflex tachy, orthostasis |
| Reversible α | Phentolamine | Short α blockade | Catecholamine crisis, extravasation | Tachycardia, ischemia in CAD |
| Selective α1 | Prazosin, Tamsulosin | ↓ SVR, relax prostate | HTN (2nd line), BPH LUTS | First-dose syncope, dizziness |
| β1-selective | Metoprolol, Atenolol | ↓ HR/contractility | Angina, AF rate, post-MI | Brady, AV block, fatigue |
| Nonselective β | Propranolol | β1+β2 block | Portal HTN, thyrotoxicosis | Bronchospasm, mask hypoglycemia |
| Mixed α1/β | Labetalol, Carvedilol | ↓ SVR with limited reflex | HF (carvedilol), dissection | Hypotension, dizziness |
Exam pearl: in catecholamine excess states (pheochromocytoma, cocaine toxicity), avoid isolated β blockade—unopposed α stimulation worsens vasoconstriction. If a β blocker is used for severe tachyarrhythmia in these contexts, it should be with concurrent α blockade or a mixed agent (e.g., labetalol), though first-line strategies often prioritize benzodiazepines and vasodilators in toxin cases.
5) Cholinergic Drugs, Antimuscarinics, and Classic Toxidromes
Direct muscarinic agonists (bethanechol, carbachol, pilocarpine) increase smooth muscle tone and glandular secretion. Bethanechol treats postoperative/neurogenic ileus and urinary retention (M3-mediated contraction of detrusor). Pilocarpine increases outflow in glaucoma (M3 on ciliary muscle opens trabecular meshwork) and stimulates salivation in Sjögren syndrome. Indirect agonists (AChE inhibitors) increase endogenous ACh: neostigmine (reverses nondepolarizing neuromuscular blockade, treats ileus/urinary retention, myasthenia), pyridostigmine (long-term myasthenia), edrophonium (historical diagnosis), and physostigmine (tertiary amine that crosses BBB—antidote for antimuscarinic delirium).
Organophosphates (e.g., parathion, malathion, nerve agents) irreversibly inhibit AChE via phosphorylation; “aging” of the bond makes inhibition permanent. Presentation: the DUMBBELSS muscarinic syndrome + nicotinic features (weakness, fasciculations) and central effects (confusion, seizures). Treatment is atropine for muscarinic symptoms and pralidoxime (2-PAM) to regenerate AChE (most effective before aging). Diazepam may be needed for seizures.
Antimuscarinics oppose M receptors. Atropine treats bradyarrhythmias and secretory/bronchial manifestations of cholinergic excess, dilates pupils (mydriasis, cycloplegia), and reduces GI motility. Ipratropium/tiotropium are inhaled M3 antagonists for COPD/asthma (less central effects). Scopolamine prevents motion sickness (vestibular M1). Benztropine/trihexyphenidyl relieve tremor/rigidity in Parkinson disease by rebalancing striatal ACh–DA tone.
| Syndrome | Dominant Receptor | Key Signs | Antidote/Countermeasure | Board Clues |
| Cholinergic excess (AChE-I) | M & N | DUMBBELSS + weakness | Atropine + Pralidoxime | Farmer/pesticide, pinpoint pupils, bronchorrhea |
| Antimuscarinic toxicity | M blocked | “Dry, hot, red, blind, mad” | Physostigmine (careful), cooling, fluids | Elderly w/ OTC antihistamine, delirium, mydriasis |
| Muscarinic agonism | M stimulated | Miosis, brady, bronchospasm, GI cramps | Atropine | Postoperative ileus/urinary retention treated by bethanechol |
| Nm blockade (phase II) | Nm desensitization | Flaccid paralysis | Supportive; neostigmine reverses nondepolarizers | Succinylcholine vs rocuronium distinction |
High-yield cautions: avoid antimuscarinics in closed-angle glaucoma and with caution in BPH. Physostigmine is appropriate in pure antimuscarinic delirium but contraindicated in TCA overdose due to risk of asystole/seizures. In myasthenia gravis crisis, differentiate myasthenic (under-treated) from cholinergic (excess AChE-I) clinically; edrophonium is historical—modern stems favor bedside reasoning (pupil size, muscarinic signs, timing with medication adjustments).
6) Baroreflex Integration: Predicting Reflex Tachycardia/Bradycardia Like a Pro
The carotid sinus and aortic arch baroreflexes stabilize MAP through rapid, powerful adjustments to vagal and sympathetic outflow. Increased stretch (↑ MAP) raises afferent firing (CN IX and X), enhancing vagal tone to the heart and suppressing sympathetic vasoconstriction—hence bradycardia and vasodilation. Decreased stretch (↓ MAP) has the opposite effect. Nearly all vasoactive stems therefore require you to separate direct drug effects from reflex responses. Pure α1 agonism (phenylephrine) raises MAP directly → reflex bradycardia; pure β2 vasodilation (isoproterenol’s vascular component) lowers MAP → reflex tachycardia, which stacks with direct β1 chronotropy.
Pitfalls cluster around mixed-profile drugs and preexisting autonomic states. Norepinephrine raises MAP so much that baroreflex-mediated vagal firing may outweigh its direct β1 chronotropy, producing an HR that is unchanged or even lower—this is not a contradiction but an integration. Epinephrine’s dose dependence explains why low-dose infusions may reduce diastolic pressure (β2 vasodilation) with tachycardia, whereas high-dose boluses increase MAP with modest HR changes.
Another layer is regional blood flow. β2-mediated dilation in skeletal muscle improves flow despite a slight drop in MAP; α1 drugs may reduce mucosal blood flow (useful for hemostasis with local anesthetics). Orthostatic hypotension from α1 blockers reflects impaired reflex vasoconstriction upon standing; elderly patients and those on PDE5 inhibitors are particularly vulnerable. Ganglionic blockers (historical but testable) eliminate reflex arcs entirely—drug effects on MAP become exaggerated because autonomic buffering is removed.
| Stimulus | Immediate Vascular Effect | MAP | Reflex Change | Net HR | Exam Cue |
| α1 agonist (phenylephrine) | Vasoconstriction | ↑↑ | ↑ vagal, ↓ sympathetic | ↓ | Mydriasis w/o cycloplegia, nasal decongestant |
| β2 agonist (isoproterenol component) | Vasodilation | ↓ | ↓ vagal, ↑ sympathetic | ↑↑ | Wide pulse pressure, tremor |
| NE infusion | Vasoconstriction + inotropy | ↑↑ | Strong reflex brady | ↔/↓ | Sepsis vasopressor; cool extremities |
| Epi (low dose) | β2 > α1 | ↘ | Reflex tachy | ↑ | Anaphylaxis logic (β2 airway) |
| Epi (high dose) | α1 dominates | ↑ | Reflex brady | ↔/↓ | Local hemostasis with lidocaine |
In summary, decide the sign of MAP change first, then add the reflex. Only override the reflex if the drug strongly drives HR directly (potent β1 agonist) or if autonomic buffering is impaired (elderly, neuropathy, ganglionic block). This simple two-step algorithm prevents most errors on ANS stems.
7) Clinical Applications, Comorbidities, and Contraindication Logic
Shock states. In septic/distributive shock, norepinephrine is favored to restore MAP via α1 with β1 support; add vasopressin for catecholamine-resistant vasoplegia (V1). Cardiogenic shock prioritizes improving CO: dobutamine or low-dose dopamine may augment inotropy, with careful afterload management. In anaphylaxis, epinephrine is first-line because it addresses three problems simultaneously: airway edema/bronchospasm (β2), distributive vasodilation (α1), and hypotension with impaired CO (β1).
Respiratory disease. β2 agonists relieve bronchospasm; LABAs require inhaled steroids in asthma. Nonselective β blockers can exacerbate bronchoconstriction and should be avoided in uncontrolled asthma; if a β blocker is necessary (e.g., post-MI), choose a β1-selective agent and monitor closely. Antimuscarinics (ipratropium/tiotropium) are excellent bronchodilators in COPD due to vagally mediated bronchoconstriction.
Cardiovascular comorbidity. β blockers improve survival post-MI and in HFrEF (carvedilol/metoprolol succinate/bisoprolol). Avoid ISA agents in ischemic heart disease. In pheochromocytoma, give α blockade before β blockade to prevent unopposed α vasoconstriction. In aortic dissection, reduce shear with β blockade (labetalol or esmolol) before vasodilators. For BPH with LUTS, α1 blockers improve flow; if a patient reports disabling dizziness or near-syncope, consider more uroselective tamsulosin or dose at bedtime.
Endocrine/metabolic. Nonselective β blockers mask adrenergic hypoglycemia warnings (tremor, palpitations) and impair hepatic glucose output; sweating (cholinergic) may still occur. Hyperthyroidism’s adrenergic symptoms respond to propranolol, which also blunts peripheral T4→T3 conversion at higher doses.
Ophthalmology & GU. Muscarinic agonists (pilocarpine, carbachol) increase trabecular outflow in glaucoma but cause brow ache and myopia; β blockers (timolol) decrease aqueous production. For overactive bladder, mirabegron (β3) relaxes detrusor; antimuscarinics (oxybutynin, tolterodine) reduce urgency but may provoke dry mouth/constipation and confusion in the elderly.
Drug–drug interactions and cautions. MAOIs or cocaine with exogenous catecholamines amplify pressor responses; tricyclics blunt reuptake and can alter expected magnitude/duration. Atropine may worsen hyperthermia by blocking sweating, particularly in hot environments. Elderly patients are exquisitely sensitive to central anticholinergics (delirium, falls); prefer peripherally restricted agents. PDE5 inhibitors plus α1 blockers or nitrates can precipitate severe hypotension—space dosing and counsel aggressively.
8) Board-Style Associations, Mini-Vignettes, and Rapid-Review Checklist
Classic Mini-Vignettes
- Anxious teen with wheeze after PE class; nebulized drug improves air entry but causes tremor and palpitations → β2 agonist (albuterol); anticipate ↓K⁺ and reflex tachy.
- Septic patient on high-dose NE develops cool, mottled extremities; HR 58 → baroreflex overcomes β1 → NE is correct pressor; bradycardia is not paradoxical.
- Farmer with pinpoint pupils, bronchorrhea, muscle fasciculations; treat muscarinic signs first with atropine, then give pralidoxime promptly to regenerate AChE.
- Elderly man starts prazosin for BPH; first-dose syncope after standing at night → orthostatic hypotension from α1 blockade; mitigate with bedtime dosing or switch to tamsulosin.
- Local anesthetic with epinephrine extravasates; blanched digit → reverse with phentolamine infiltration (α blockade).
Reflex Outcomes: One-Liners
- ↑MAP → reflex bradycardia (phenylephrine, high-dose epi, NE).
- ↓MAP → reflex tachycardia (isoproterenol, pure vasodilators).
- β-blocker + epinephrine → unopposed α → hypertensive crisis.
- Antimuscarinic toxidrome → hyperthermia, mydriasis, dry skin (no diaphoresis).
- DUMBBELSS points to AChE inhibition—treat with atropine ± pralidoxime.
Rapid-Review Checklist
- Couplings: Gq (α1/M1/M3), Gi (α2/M2), Gs (β1/β2/β3). Nicotinic = ligand-gated Na⁺/K⁺.
- Eye: α1 → mydriasis (no cycloplegia); M3 → miosis + accommodation.
- Heart: β1 → ↑ HR/contractility; M2 → ↓ HR/AV conduction.
- Vessels: α1 → constrict; β2 → dilate (skeletal muscle beds).
- Lungs: β2 → bronchodilate; M3 → bronchoconstrict + secretions.
- Bladder: M3 → detrusor contracts (urination); β3 → relaxes (storage); α1 → sphincter tightens.
- Pressors: NE for sepsis; epi for anaphylaxis; phenylephrine for pure vasoconstriction needs.
- Contraindications: Nonselective β blockers in asthma; antimuscarinics in closed-angle glaucoma; β-blocker alone in catecholamine excess.
- Antidotes: Organophosphate → atropine + pralidoxime; antimuscarinic delirium → physostigmine (avoid in TCA overdose).
| Toxidrome | Dominant Signs | Key Antidote(s) | Do-Not-Miss |
| Organophosphate | DUMBBELSS, miosis, bronchorrhea, weakness | Atropine + Pralidoxime | Early 2-PAM before “aging” |
| Antimuscarinic | Hyperthermia, anhidrosis, mydriasis, delirium | Physostigmine (if pure), cooling | Avoid in TCA overdose |
| β-blocker overdose | Bradycardia, hypotension, hypoglycemia | Glucagon, high-dose insulin, atropine | Masking of hypoglycemia symptoms |
References
- Katzung BG, Trevor AJ. Basic & Clinical Pharmacology. McGraw-Hill Medical. accessmedicine.mhmedical.com
- Brunton LL et al., eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. McGraw-Hill. accessmedicine.mhmedical.com
- StatPearls (NCBI Bookshelf): “Adrenergic Receptors”, “Beta Blockers”, “Anticholinergic Toxicity”, “Organophosphate Toxicity”. ncbi.nlm.nih.gov/books
- Merck Manual Professional Edition: Autonomic Nervous System Overview & Drug Toxicities. merckmanuals.com
- OpenAnesthesia: Vasoactive Drugs (phenylephrine, epinephrine, norepinephrine). openanesthesia.org
100+ new students last month.