Use the current NBME Step 1 interactive practice (“Free 120”) to sharpen exam-day logic. Below: concise “why right/why wrong” rationales by theme, common traps to avoid, and links to the official interface and content specs. Where we suggest Q-bank or flashcards, assume
MDSteps tools (Adaptive QBank >9,000 items, auto flashcards from misses, AI tutor, analytics, and dynamic
study plan).
Make the Free 120 Work for You: Setup, Run, and Scoring Expectations
The NBME Free 120 is delivered in an interface that closely mirrors the real testing platform: same navigation, flagging, exhibits, labs, and calculator behavior. Launch the Step 1 orientation and practice blocks in a single sitting with the timer enabled to simulate cognitive load and pacing. Doing this preserves the fidelity of your metrics—time per question, flag behavior, and end-of-block review—so your performance generalizes to test day.
Expect seven 60-minute blocks on the real exam (≤40 questions each; ≤280 total). While the Free 120 uses three blocks, aim for the same per-item tempo (~90 seconds) and practice your micro-break routine between blocks. If you enable the tutorial on exam day, it can be converted into additional break time—rehearse that timing choice now so it’s automatic later.
Run protocol: (1) One warm-up item (low stakes) to settle nerves. (2) Commit to a 60–90–120s triage ladder: quick wins first, defer deep reads. (3) Flag only for revisitable uncertainty (calculation, 2 plausible keys) rather than generic “review later.” (4) End-of-block: review flags and any ≤15-second rechecks; avoid wholesale re-reads that create decision churn. This preserves attention for subsequent blocks and approximates live constraints.
Scoring expectations: Don’t over-interpret a single sitting. The Free 120 samples common Step 1 patterns but is shorter than the full exam, and items may lag current content emphases. Use errors to identify process failures (misread lead-in, missed negation, premature closure) as much as content gaps. Then translate each miss into a drillable task (see Section 7). For content breadth/weighting, anchor to the official Step 1 outline and competency ranges.
| Step | Action | Why it matters |
|---|
| Before | Enable timer; full-screen; scratch paper + noise plan | Mimics cognitive environment |
| During | 60–90–120s triage; precise flagging | Protects points/time under uncertainty |
| After | Review flags + 15-sec rechecks only | Reduces second-guess fatigue |
Fast “Why Right/Why Wrong”: A Board-Style Elimination Framework
Treat each vignette as a closed-stem diagnostic: the correct key is supported by converging data; distractors are made plausible by one feature but contradicted by the totality. Start with the lead-in (“Which of the following is the most likely diagnosis/mechanism/next step?”) and predict an answer category before viewing options. Then interrogate options with three passes: Screen for category mismatch; Challenge with must-be-true criteria; Confirm by locating the stem sentence that uniquely supports the survivor. This mirrors NBME item-writing logic (focused lead-ins, homogeneous options, removal of technical cues).
Micro-rationales that unlock items: (1) Mechanism vs. manifestation: If the lead-in asks for mechanism, penalize option choices that are diagnoses or therapies—even if clinically tempting. (2) First-order beats second-order: Prefer directly evidenced physiology/pathology over downstream associations unless the prompt explicitly demands a consequence. (3) Necessary finding test: For each candidate key, name the necessary stem fact; if absent, discard. (4) Temporal anchors: Acute vs. chronic, neonatal vs. adolescent, immediate vs. delayed hypersensitivity—time words carry the question.
Common distractor props: (a) Red-herring labs with mild deviations that are clinically irrelevant; (b) Binary traps (“always/never,” “pathognomonic”) that don’t tolerate physiologic variation; (c) Medication misattribution—confusing intended effect with adverse effect; (d) Mechanistic near-misses (e.g., confusing enzyme inhibition with decreased gene transcription). These exist because good items keep all options plausible yet clearly wrong when weighed against the stem. Practice verbalizing the single disconfirming fact for each eliminated distractor to cement the logic.
Finally, self-test this elimination sequence—not passive rereads—to lock retrieval routes and reduce race-day latency (testing effect). Build a habit of writing a five-to-ten-word rationale for your selected key and a single killer reason each distractor fails; this produces robust memory traces and speeds future eliminations.
Biostats & Ethics: Highest-ROI Pitfalls and 60-Second Fixes
Study design → best test: Map vignette language to the inferential tool. Case–control → odds ratio; cohort → risk difference/relative risk; RCT → intention-to-treat effect; diagnostic accuracy → sensitivity/specificity/likelihood ratios; screening → PPV/NPV dependence on prevalence. Build a “trigger phrase” lexicon (e.g., “retrospective, rare outcome” → case–control). Then compute minimally: structure a 2×2 table first; derive OR = ad/bc, RR = [a/(a+b)] / [c/(c+d)], NNT = 1/ARR. Keep units consistent and beware denominator swaps.
Common traps: (1) Base-rate neglect—PPV rises with prevalence; low-prevalence screens make false positives dominate. (2) Verification bias—gold standard applied selectively inflates sensitivity/specificity. (3) Multiple comparisons without correction—spurious “significant” findings. (4) Non-inferiority margins misread as equivalence. (5) Confidence interval that crosses the null (1.0 for ratios; 0 for differences) indicates “not significant.”
Ethics heuristics (Step 1 level): Prioritize patient safety and autonomy. If a question pits curiosity versus safety, choose the action that prevents harm first (e.g., halt a faulty protocol; disclose error; obtain consent). When confidentiality conflicts with safety (e.g., imminent harm to others), choose the exception path. If capacity is in question, assess and document; if absent, use the appropriate surrogate hierarchy. These priorities align with physician tasks/competencies emphasized on Step 1 (Communication, Practice-based Improvement).
| Pitfall | Red Flag in Stem | One-Line Fix |
|---|
| PPV/NPV error | “Rare disease; screening test positive” | Re-compute with prevalence-aware 2×2 |
| OR vs. RR swap | “Retrospective case–control” | Use OR only; RR undefined |
| CI misread | “95% CI 0.8–1.3 for RR” | Crosses 1 → not significant |
| Verification bias | “Gold standard for positives only” | Bias inflates test accuracy |
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
High-Frequency Clinical Science Themes: Quick Rationales & Miss Patterns
Microbiology: Tie organism to exposure + virulence + host. Quick keys: Catalase+/coagulase+ cocci with acute device infections → S. aureus (protein A, abscess-forming); alpha-hemolysis, optochin-sensitive with lobar consolidation → S. pneumoniae; gram-negative oxidase+ comma-shaped with rice-water stools → V. cholerae (Gs activation → ↑cAMP). Pitfall: over-weighting single lab while ignoring exposure or immune status.
Immunology/Path: Distinguish mechanism (Type II vs. III vs. IV) from manifestation. Linear immunofluorescence hemoptysis + renal failure → anti-GBM (Type II, complement-mediated); post-strep glomerulonephritis → immune complex (Type III); contact dermatitis → T-cell mediated (Type IV). One-liner: mechanism asks “what immune process?” not “what disease name?”
Pharmacology: For adverse effects, categorize by on-target vs. off-target and dose-dependence. Aminoglycosides → dose-dependent nephro/ototoxicity (accumulation in proximal tubules/hair cells); non-dihydropyridine CCBs → bradycardia/AV block (on-target cardiac conduction). Trap: confounding drug class cousins (e.g., β1-selective vs. nonselective β-blockers) when the stem hinges on comorbid asthma or variant angina.
Genetics/Biochem: Recognize inheritance signatures (vertical transmission autosomal dominant; maternal lineage mitochondrial). For inborn errors: think bottleneck metabolite + organ predilection (ammonia for urea cycle → neurologic; odd-chain FA for propionic acidemia → anion gap metabolic acidosis). In enzyme questions, the wrong choices often describe adjacent steps—write the substrate/product pair to expose the near-miss.
Weighting of systems and tasks is specified in the Step 1 outline—helpful to calibrate your practice mix when building custom blocks (e.g., 60–70% foundational science application; 20–25% diagnosis). Use this to align your Free 120 post-hoc drills with exam emphasis.
Data-Heavy Stems: Tables, Graphs, and Imaging Without Getting Stuck
Three-pass parse: Pass 1: Title/axes/units to define the question’s “universe.” Pass 2: Identify the contrast (treatment vs. control, pre- vs. post-, mutated vs. wild-type). Pass 3: Extract only the decision-critical deltas (direction > magnitude). Many misses occur because examinees read every cell instead of comparing the two cells that change the answer.
Lab tables: Normalize first: convert to the same unit family; mark path-defining thresholds (e.g., anion gap; corrected calcium). If the lead-in is mechanistic (enzyme up/down; receptor signaling), translate the lab pattern into pathway arrows before hunting options. For conflicting labs, prioritize pathognomonic pairs (e.g., ↑indirect bilirubin + ↑LDH + ↓haptoglobin → hemolysis) over single outliers.
Imaging/Path photos: Identify organ → pattern → qualifier. “Lung → peripheral, wedge-shaped opacity” suggests pulmonary infarct; “kidney → subepithelial humps on EM” points to post-strep GN. When two patterns look alike, anchor on demographics/time course to break ties (acute vs. chronic, child vs. adult).
Time saver: If a figure is dense, skip to the caption, then the question, then return for a targeted read. This is legitimate on the Free 120 and the live exam, where you must balance depth with the 60-minute block budget. Rehearsing this pattern in the interactive sample questions acclimates you to the toolchain (zoom, exhibits, lab pop-outs).
Algorithm: 45-Second Table Decode
- Circle the comparison (row/column pairs that change the answer).
- Mark unit mismatches; convert once mentally.
- Translate pattern → mechanism → shortlist 2 keys.
- Kill each distractor with a single contradictory cell.
Pacing & Triage: Protecting Points Under the 60-Minute Clock
Step 1 allocates ≤40 items per 60-minute block. Aim for an average of ~90 seconds per item, deliberately finishing straightforward questions in ~60 seconds to “bank” time for computational or exhibit-heavy vignettes. Use a pre-committed triage ladder: (A) 60s quick solve → select and move; (B) 90s wrestle → if not cracked, flag with a two-word reason (“calc,” “2 keys”); (C) 120s stop → prevent time sink. Practice this in the NBME interface to habituate the motor sequence of flag-and-advance.
When to skip early: (1) Multi-exhibit questions where you haven’t previewed the lead-in; (2) Dense lab figure with mixed units; (3) Calculations without a set 2×2 skeleton yet; (4) Two plausible mechanistic keys you can’t separate without a careful reread. Skipping earlier preserves tempo and reduces downstream panic.
Flag discipline: Flags are not emotional placeholders; they are specific plans. “Calc” = return with a filled 2×2; “Imaging” = return after completing content-first items; “2 keys” = hunt for the unique must-be-true stem line. End-of-block reviews should focus purely on flagged items plus sub-15-second sanity checks.
| Scenario | Action in 10s | What you gain |
|---|
| Lead-in unclear | Read lead-in first, predict category | Prevents option-driven anchoring |
| Calc w/o 2×2 | Draw 2×2; place givens; return | Accuracy > speed |
| Two plausible keys | Flag “2 keys”; resume flow | Maintains block rhythm |
| Data-dense exhibit | Caption → question → targeted scan | Time control |
Turning Misses into Mastery: A Concrete Post-Free-120 Workflow
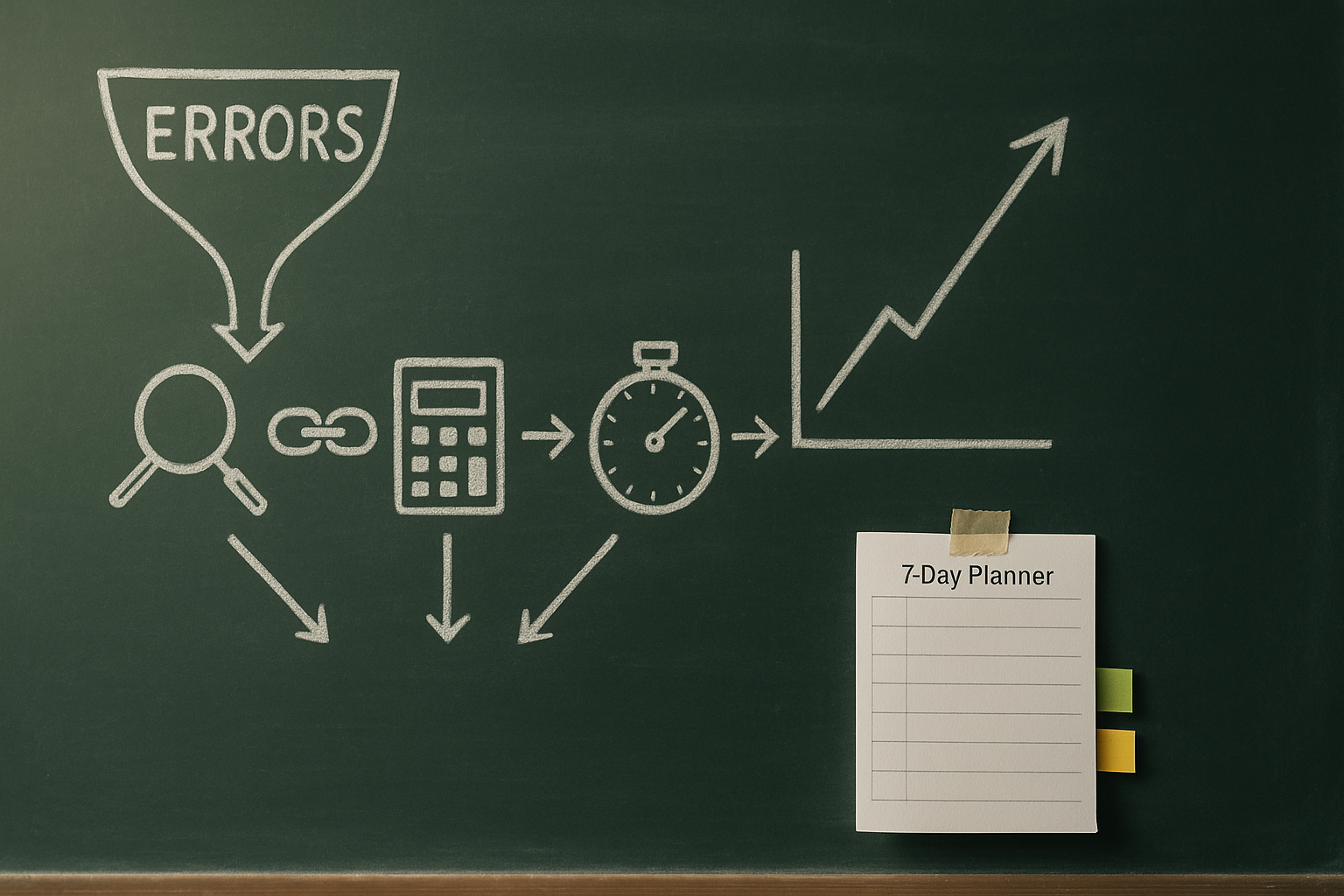
The biggest ROI from the Free 120 comes after you submit. For each miss, write two lines: (a) the specific decision error (e.g., “misread lead-in asks mechanism, I answered diagnosis”), and (b) the one-sentence mechanistic rationale for the correct key. Then route the miss through an evidence-based loop: immediate test-enhanced review (self-explain choice architecture), a next-day retest, and a spaced reprise at 7–10 days. Spacing + retrieval beats reread-and-highlight every time.
| Miss Type | Example | MDSteps Action | Outcome |
|---|
| Lead-in mismatch | Asked “mechanism,” answered diagnosis | AI tutor generates contrast set (mechanism vs. manifestation) + micro-quiz | Faster cue recognition |
| Biostats arithmetic | OR vs RR swap | Adaptive QBank block with mixed 2×2 builds; on-board calculator drills | Reduced compute latency |
| Content gap | Complement pathways | Auto flashcards from your miss; exported to Anki; spaced via study plan | Long-term retention |
| Time sink | Over-reading exhibits | Timed mini-blocks; analytics on per-item time & flag rate | Stable pacing |
Use the MDSteps analytics dashboard to tag each miss by system, task (diagnosis, mechanism), and cognitive error. The automatic study plan generator will then schedule mixed-difficulty reinforcement aligned with the official content outline—keeping rehearsal aligned to Step 1 priorities while you clear specific error patterns.
Curated Links: Official Free 120, Interface Practice, and Specs
For readiness checks beyond the Free 120, NBME self-assessments (CBSSA) provide scaled feedback and trendable subscores; use them to calibrate your remaining study weeks and to verify that your Free 120-derived fixes are sticking.
Top 12 Pitfalls on the Free 120 (and the Live Exam)—with Fast Fixes
- Answering the wrong question. Read the lead-in first; restate it in your own words. (Mechanism ≠ diagnosis.)
- Over-reading normal variants. Mild lab skews that don’t change management are distractors—seek path-defining pairs.
- RR vs OR confusion. Build the 2×2; case–control uses OR.
- Forgetting prevalence in PPV/NPV. Anchor PPV/NPV to disease prevalence.
- Verification bias blind spot. Gold standard applied only to positives inflates accuracy.
- Premature closure. Two plausible keys? Flag and return with a “must-be-true” test.
- Time sink on figures. Caption → lead-in → targeted read; don’t scan every cell first.
- Ethics misprioritization. Safety and autonomy first; document capacity.
- Mechanism/manifestation swap. When asking for mechanism, penalize “diagnosis” options unless specifically requested.
- Confusing on-target with off-target drug effects. Classify the adverse effect before selecting.
- Negation misses. “Except/Not/Least” should trigger a slow-down pass.
- No retrieval loop after review. Don’t just reread; retest with spaced intervals.
Rapid-Review Checklist: One-Page Run-Through Before You Launch
- Environment: Timer on, full-screen, quiet space, snacks/water staged.
- Tempo: Target 60–90–120s triage with disciplined flags.
- Lead-in first: Predict category before viewing options.
- Data items: Caption → question → critical deltas; convert units once.
- Biostats: 2×2 first; OR for case–control; check CI vs. null.
- Ethics: Safety/autonomy; document capacity; use surrogate if needed.
- Post-hoc loop: Two-line miss log → MDSteps auto cards → spaced retest (1d, 7–10d).
- Analytics: Tag by system/task/error; schedule adaptive blocks to match Step 1 specs.
Your MDSteps Toolkit (Step 1)
- Adaptive QBank (>9,000) with custom mixed blocks
- Auto flashcards from misses (export to Anki)
- AI tutor for contrast sets & quick rationales
- Analytics dashboard: time/item, system, task
- Automatic study plan generator (aligns to USMLE specs)
10-Day Mini-Plan After Free 120
- Day 1: Miss log + 2×2 biostats clinic
- Days 2–3: Mixed MDSteps blocks from weak systems
- Days 4–5: Mechanism vs. manifestation drills
- Day 6: Data-heavy exhibits practice
- Day 7: Ethics/communication micro-sets
- Day 8: Timed blocks + flag discipline
- Day 9: Retest your miss set
- Day 10: Readiness check & plan adjustments
References & Official Resources
100+ new students last month.