Compare the best Step 3 CCS cases platform—MDSteps, CCSCases.com, UWorld, and others—ranked by realism, feedback, and test-day transfer, plus a training plan.
USMLE Step 3
CCS strategy
Updated: Feb 8, 2026
What you’ll get
- A transparent ranking rubric (realism, physiology, feedback, and UX)
- A head-to-head table across major simulators (MDSteps, CCSCases.com, UWorld, more)
- Purchase scenarios for interns, IMGs, and last-minute testers
- A 14-day practice plan and an exam-day checklist
Why your CCS simulator choice matters more than your case count
If you’re searching for the best Step 3 CCS cases platform, you’re already asking the right question—but the
“best” option is rarely the one with the most cases. On Step 3, Computer-based Case Simulations (CCS)
reward sequencing, timing, and setting (clinic vs ED vs inpatient) as much as diagnosis.
A platform that forces you to practice those mechanics—free-text order entry, deliberate clock management,
and physiologic consequences—usually transfers better to test day than passive reading or static checklists.
The USMLE describes CCS as a dynamic simulation where patient status changes with simulated time and with
your management choices. You’re scored on indicated actions, their timing and sequence, and you lose points
for unnecessary or harmful actions. In other words: the “right” order late can be worth little, and the
“reasonable” order placed in the wrong setting can silently drag you down.
What CCS is actually testing
- Stabilize first (ABCs, immediate threats, correct disposition)
- High-value diagnostics that change management
- Therapy + monitoring with correct time advancement
- Stop rules: when observation beats “more testing”
- Safe discharge: follow-up, counseling, and prevention when relevant
What CCS platforms should train (but many don’t)
- Clock discipline: advance time only when you expect results or updates
- Order batching: place critical orders together to avoid time waste
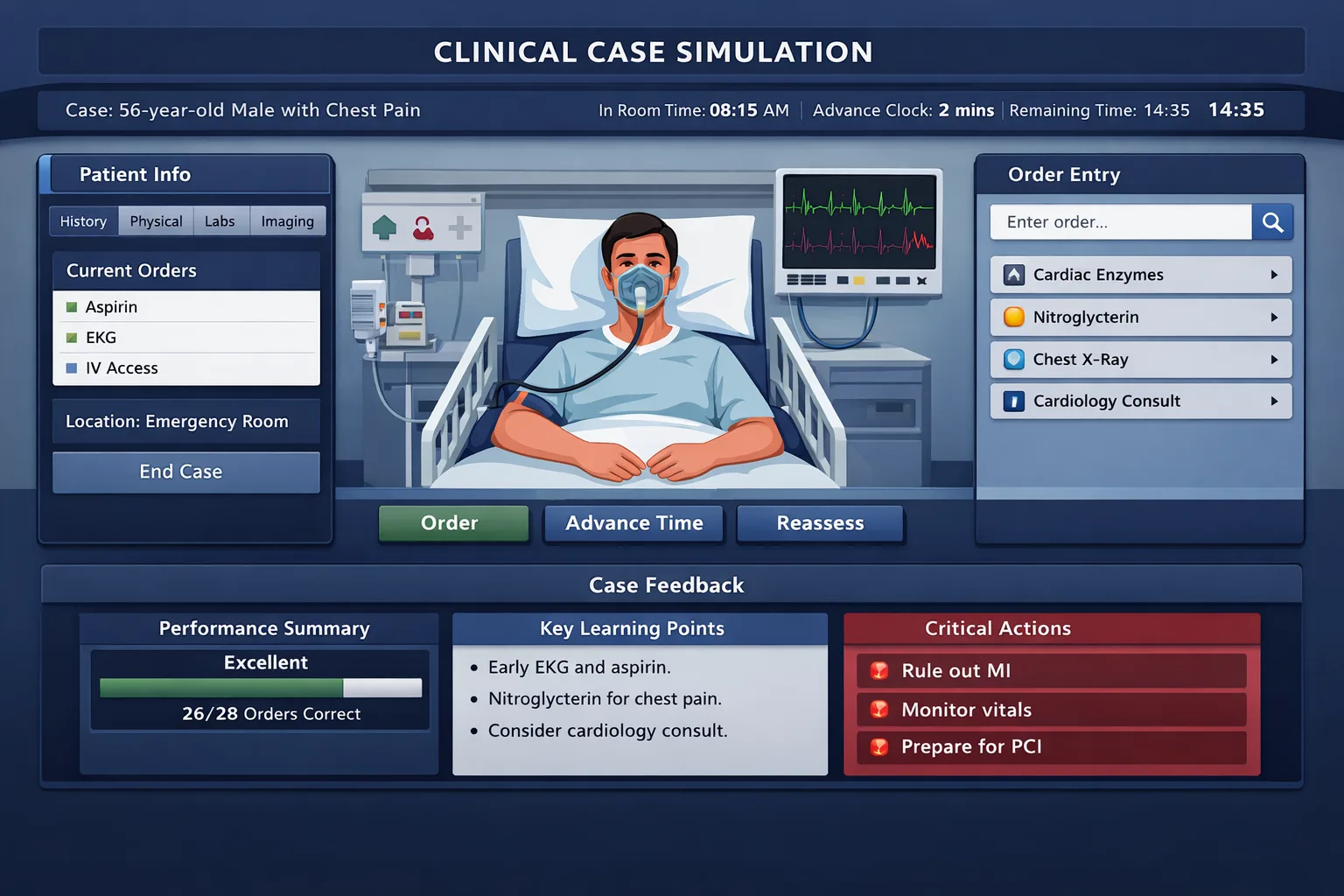
- Physiology feedback loop: vitals/labs improve or worsen based on your actions
- Interface fluency: the fewer “where is that button?” moments, the better
- Actionable debrief: why you lost points and what to do differently next time
Board-style trap: CCS punishes “smart-looking” over-ordering.
The higher your anxiety, the more likely you are to reflexively order broad panels and unnecessary imaging.
A strong simulator doesn’t just show what to order—it trains restraint and sequencing.
A practical ranking rubric: the 6 features that predict test-day transfer
CCS platforms differ most in how they teach you to think under the clock. To compare them fairly,
this article uses a rubric built around the components the USMLE emphasizes: appropriate actions, correct
setting, and correct timing/sequence. We also weigh usability and feedback quality because they determine
whether you can iterate quickly across many cases.
| Rubric domain |
What “excellent” looks like |
Why it matters on Step 3 |
| Interface fidelity |
Free-text ordering, realistic chart layout, clock controls, and case-end behavior that feels like Primum. |
Reduces cognitive load so you can focus on management rather than software navigation. |
| Physiology realism |
Vitals/labs respond plausibly to interventions and time; wrong moves create believable deterioration. |
Forces “treat → reassess → advance time” loops that match CCS scoring logic. |
| Scoring transparency |
Clear breakdown of points: diagnosis, therapy, monitoring, timing/sequence, and setting. |
Lets you fix the true problem (eg, correct order but late; correct treatment but wrong setting). |
| Debrief actionability |
Shows missed high-yield orders, harmful/unnecessary actions, and a better sequence you can rehearse. |
Turns each case into a repeatable algorithm instead of a one-off “gotcha.” |
| Case breadth + curation |
Core emergencies + ambulatory care + inpatient management; minimal redundancy. |
Prevents overfitting to a narrow pattern set; Step 3 mixes settings and acuity. |
| Workflow + analytics |
Tracks trends across cases (missed monitoring, late antibiotics, wrong disposition) and drills weaknesses. |
CCS improvement is pattern-based; you win by eliminating recurring “silent” errors. |
How to use this rubric (fast)
- Pick the platform that best matches your weakest rubric domain.
- Do 3–5 cases, then audit your errors by domain (timing vs diagnosis vs monitoring).
- Switch or supplement only if your weak domain isn’t improving after ~10 cases.
Common CCS weaknesses the rubric will reveal
- Late life-saving therapy (eg, delayed antibiotics/anticoagulation)
- Wrong setting (admit vs observe vs discharge; ICU timing)
- Monitoring gaps (telemetry, strict I/Os, repeat vitals, reassessment)
- Over-ordering (low-value labs/imaging, shotgun consults)
- Broken time loops (advancing time without a plan for results)
Ranked comparison: major CCS simulators side-by-side
Below is a high-yield comparison of widely used CCS practice options. “Rank” reflects the rubric above and
prioritizes test-day transfer, not marketing claims. Costs and case counts can change, so treat those as
directional and verify on the vendor site.
| Rank* |
Platform |
Best for |
Strengths |
Limitations |
Quick pick |
| #1 |
MDSteps |
Students who need physiology-driven practice + analytics to fix repeat mistakes. |
Live vitals/labs responses, timed orders, outcome-based scoring, robust scorecards and trends. |
Smaller ecosystem than legacy tools; best value when used with a structured plan. |
If you miss points on timing/monitoring/disposition, start here. |
| #2 |
CCSCases.com |
High-volume repetition to build interface fluency and a broad order vocabulary. |
Large case bank, realistic feel, large order database, end-of-case grading/feedback. |
Physiology depth varies by case; analytics are more case-by-case than longitudinal. |
Great “mileage” if you can grind many cases quickly. |
| #3 |
UWorld CCS |
UWorld users who want CCS familiarity inside one subscription and strong explanations. |
Free-text order entry emphasis; educational explanations; integrates with Step 3 QBank workflow. |
Time-cost can be high; feedback may feel less granular for sequencing errors. |
Solid all-in-one if you already live in UWorld. |
| #4 |
MasterCCS |
Learners who want real-time scoring cues while working through cases. |
Emphasizes real-time scoring and detailed feedback; broad order database. |
Less “battle-tested” by large user base vs CCSCases/UWorld; verify case breadth and updates. |
Consider as a supplemental “feedback-first” option. |
| Baseline |
USMLE sample CCS |
Everyone, regardless of platform. |
Official Primum feel; calibrates your expectations for case flow and clock behavior. |
Limited number of cases; not enough alone for skill building. |
Do these early, then again in the final week. |
| Not a simulator |
AMBOSS |
QBank + knowledge gaps (Step 3 MCQ), not CCS simulation. |
Strong library and question bank workflows. |
Does not provide Step 3 CCS simulations (as of current public statements). |
Use for MCQ; pair with a CCS simulator. |
*Ranking reflects exam-transfer features (timing/sequence, setting, physiologic consequences, feedback quality).
Different budgets and timelines may shift what’s “best” for you.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
Deep dive: what each platform does well (and where it can cost you points)
A CCS simulator is only as useful as the habits it builds. This section translates platform features into
Step 3 scoring behaviors: what you’ll do faster, what you’ll stop over-ordering, and what you’ll learn to
recognize early. Use it to pick the tool that fixes your weak links.
How to choose based on your timeline: 4 common purchase scenarios
The “right” simulator depends on how much time you have and what type of errors you make. Use the scenarios
below to pick a setup that fits your constraints without overbuying. The goal is a tight feedback loop:
do a case → identify a recurring error → drill that error on the next case.
Scenario A: 10–14 days left, minimal prep time (intern schedule)
- Priority: timed performance reps + clean debrief
- Pick: one simulator + official sample cases
- Strategy: 2–3 timed cases/day, repeat the “missed pattern” case types
Rule: spend ≤5 minutes reviewing the debrief, then immediately do another case that targets the same weakness.
Scenario B: 3–6 weeks, solid knowledge but CCS anxiety
- Priority: interface fluency + clock instincts
- Pick: a high-volume simulator (for repetition) plus a feedback-rich tool (for correction)
- Strategy: alternate: “volume day” (many cases) vs “analysis day” (fewer cases, deep debrief)
Your target outcome is not “high percentage” early. It’s a steep improvement curve by week two.
Scenario C: IMG or away from clinical care
- Priority: management sequence + disposition logic
- Pick: a simulator that emphasizes physiology and setting decisions
- Strategy: build a “default order set” for ED vs inpatient vs clinic, then refine per case
Make a one-page template: ED stabilizers, inpatient maintenance orders, discharge/follow-up checklist.
Scenario D: Strong CCS, weak Step 3 MCQ
- Priority: do not overinvest in CCS; maintain skill with lighter reps
- Pick: official cases + a small set of high-yield timed cases weekly
- Strategy: shift most hours to MCQ and biostats; keep CCS “muscle memory” warm
CCS is a quarter-ish of the exam experience; you still need enough MCQ points to buffer tough cases.
MDSteps note (one-time): if you want a simulator that actively trains timing/sequence with evolving vitals and then
shows you a robust scorecard of recurring misses, MDSteps’ CCS runner is built for that feedback loop.
A 14-day CCS training plan that actually improves your score
CCS improvement is less about “learning more medicine” and more about building a repeatable, time-safe workflow.
Below is a two-week plan you can run with any simulator. The plan assumes you can do 1–3 cases/day; adjust up or
down without changing the structure: timed reps + debrief + targeted redo.
| Days |
Primary objective |
Daily case work |
Debrief focus |
| 1–2 |
Interface calibration + baseline habits |
Official sample cases + 1 timed simulator case |
Where did you lose time? What buttons/searches slowed you down? |
| 3–5 |
Emergency workflow (ABCs, disposition) |
2 timed ED cases/day (sepsis, chest pain, SOB, altered mental status) |
Did life-saving therapy happen first? Were you in the right setting? |
| 6–8 |
Inpatient management + monitoring |
2 timed inpatient cases/day (CHF, DKA/HHS, GI bleed, pancreatitis) |
Missing telemetry? repeat vitals? strict I/Os? DVT prophylaxis? |
| 9–11 |
Clinic logic + preventive care |
2 timed clinic cases/day (DM, HTN, prenatal, outpatient infections) |
Follow-up intervals, counseling, vaccines/screening where relevant |
| 12–13 |
Mixed settings + time stress |
3 timed cases/day; force yourself to finish with 2 minutes spare |
Identify top 3 recurring mistakes and write “if-then” fixes |
| 14 |
Final calibration + confidence |
Redo official cases + 1–2 “weakness” cases |
Run your checklist; practice calm pacing and close-out orders |
Your default CCS sequence (memorize this)
- Place setting + stabilizers (O2, monitors, IV access, NPO if needed).
- Batch the first diagnostic set (only what changes management).
- Treat early for high-risk conditions (don’t wait for perfect confirmation).
- Advance time to the next meaningful checkpoint.
- Reassess → adjust therapy → repeat monitoring.
- Close out with disposition + follow-up + prevention when relevant.
How to debrief in 4 minutes (no fluff)
- 1 minute: list 3 missed high-yield actions.
- 1 minute: identify the single “too late” action.
- 1 minute: identify one unnecessary/harmful action to stop doing.
- 1 minute: write a replacement script (what you’ll do first next time).
If you want this plan auto-generated around your calendar and then adjusted based on your misses, MDSteps’ platform
can build an automatic study plan and track your case-level patterns, so your practice time targets the errors that
actually cost points.
Exam-day essentials: closing orders, time traps, and what not to do
Test-day CCS is a performance task. Your goal is to look like a competent, unsupervised generalist: stabilize,
diagnose, treat, monitor, and safely disposition. The biggest point losses come from (1) late critical therapy,
(2) wrong setting, (3) missing monitoring/reassessment, and (4) wasteful over-ordering. Use the checklist below
to make your performance consistent across every case, including the weird ones.
Rapid-Review Checklist (printable)
- Start: confirm location, then place stabilizers (pulse ox, O2, cardiac monitor as appropriate, IV access).
- Focused exam: don’t waste time on a full exam in emergencies; do targeted components.
- Diagnostics: order the minimum that changes management (don’t shotgun).
- Treatment first when indicated: sepsis antibiotics/fluids, ACS aspirin/heparin when appropriate, anaphylaxis epi, etc.
- Monitoring: repeat vitals, strict I/Os, telemetry, glucose checks, reassessment after interventions.
- Disposition: admit vs ICU vs discharge with follow-up; don’t keep unstable patients outpatient.
- Close-out: meds, follow-up interval, return precautions, counseling (smoking, diet), vaccines/screening when relevant.
- Stop rules: when observation is correct, stop testing and advance time until case ends.
High-yield “don’t do this” list
- Don’t advance time “just to see what happens.” Advance to a planned checkpoint.
- Don’t order consults as a reflex. Use them only when your plan requires it.
- Don’t order broad imaging without a clinical question (and an impact on management).
- Don’t forget to reassess after giving treatment—many points live there.
- Don’t ignore harm: contraindicated meds/procedures can drop your score fast.
Time trap to anticipate: if you place orders but don’t advance the clock to the report time,
you won’t see results or treatment effects. Conversely, if you advance time with no pending results, the case
may jump forward unexpectedly. Plan your clock moves.
Bottom line recommendations and how to combine platforms efficiently
Most learners don’t need three simulators. They need one simulator that builds the right habits, the official
cases for calibration, and a plan that forces deliberate improvement. If your main weakness is software
fluency and exposure, prioritize a large case bank. If your weakness is timing, monitoring, or
disposition, prioritize physiology-driven reps and debriefs that tell you exactly what to change.
If you can only pick one
- Need feedback + physiologic realism: pick MDSteps-style cases and run the 14-day plan.
- Need maximum repetition on a budget: pick CCSCases.com and audit timing/setting deliberately.
- Already committed to UWorld: use UWorld CCS, but keep reps timed and add official cases twice.
A simple combo that works
- Week 1: official sample cases + one primary simulator (build workflow).
- Week 2: focus on your top 3 recurring mistakes (drill and redo similar cases).
- Final days: redo official cases + timed “weakness” cases only.
One-sentence CTA (keep it simple)
Want physiology-driven CCS practice with timed orders and a scorecard that shows exactly what you missed and how to fix it?
Try MDSteps’ Step 3 CCS cases alongside your QBank and run the 14-day plan above.
Citations & external references
Medically reviewed by: Jennifer L. Nguyen, MD
100+ new students last month.