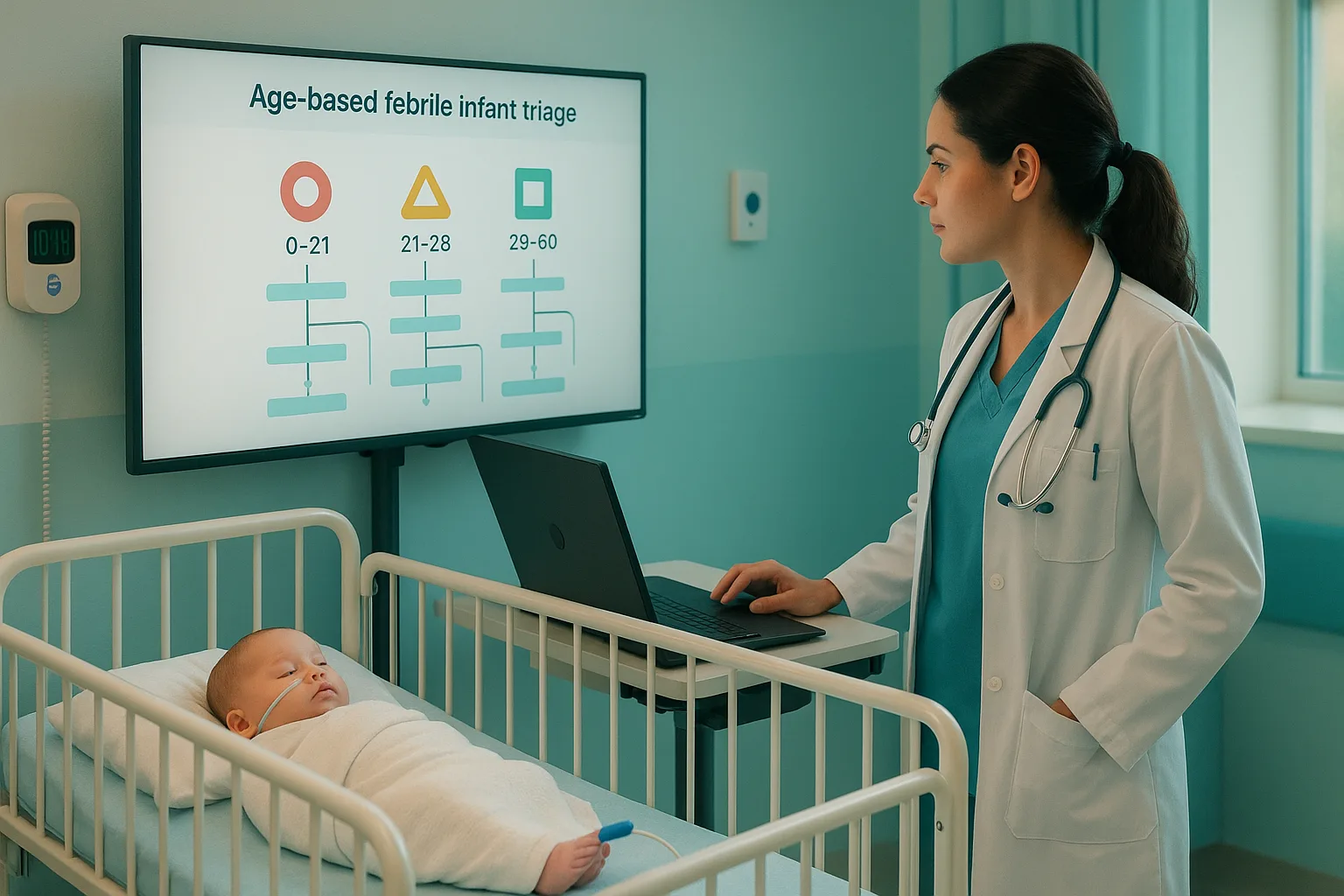
Shortness of breath on the USMLE is designed to test whether you can quickly separate immediately life-threatening diseases from conditions requiring targeted but non-emergent management. This article breaks down a high-yield shortness of breath differential algorithm that distinguishes pulmonary embolism, acute decompensated heart failure, COPD exacerbation, and pneumonia—four of the most frequently tested etiologies. Early within any vignette, note whether the patient appears toxic, unstable, or in obvious respiratory distress, because the exam expects stabilization before diagnostic workup. Also pay attention to clues such as fever, wheezing, orthopnea, pleuritic pain, or unilateral leg swelling; these distinguish key branches of the differential within the first 30 seconds of reading. Exam writers repeatedly recycle patterns: sudden-onset dyspnea with clear lungs favors PE, diffuse crackles plus volume overload points to CHF, purulent sputum with fever suggests pneumonia, and wheezing with hypercapnia usually indicates COPD exacerbation. The algorithm below is built around NBME logic—starting with acuity, then lung exam, then perfusion, and finally targeted diagnostics. Mastering this flow reduces cognitive load and improves pattern recognition, especially during long “mixed block” Step 2 CK and Step 3 sessions. The most efficient dyspnea algorithm uses a three-step approach: stabilize, separate emergent causes, then solve the rest. For USMLE purposes, stabilization means assessing oxygen saturation, mental status, work of breathing, and hemodynamics. Any patient who is hypoxic, altered, or hypotensive requires oxygen support first—then diagnostics. Once stable, separate causes using three high-yield filters: USMLE vignettes also incorporate lab “triads”: PE often shows mild respiratory alkalosis; CHF shows elevated BNP; COPD shows hypercapnia with compensatory bicarbonate elevation; pneumonia shows leukocytosis and infiltrates. Integrating these filters produces rapid diagnostic certainty even before imaging. Pulmonary embolism is one of the highest-stakes conditions on the exam due to its rapid onset, its potential for hemodynamic collapse, and the need to choose the correct next step. Any presentation involving sudden shortness of breath, pleuritic chest pain, tachycardia, hypoxia, and normal lung exam should immediately trigger suspicion. USMLE writers often plant additional clues: unilateral leg swelling, recent surgery, cancer, immobilization, pregnancy, or estrogen therapy. Initial tests include ECG (sinus tachycardia is most common), CXR (usually normal), and ABG (respiratory alkalosis). For low–intermediate suspicion and normal vitals, D-dimer is appropriate. For moderate–high suspicion or instability, CT angiography is the standard next step unless contraindicated. In pregnancy or renal failure, V/Q scanning is preferred. Hemodynamically unstable patients with suspected PE require immediate anticoagulation and consideration of thrombolysis before definitive imaging if instability persists. Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data. Acute decompensated heart failure presents with dyspnea, orthopnea, PND, elevated JVP, bilateral crackles, and peripheral edema. Hypertension, arrhythmias, ischemia, anemia, or non-compliance with medications are common precipitating factors. The hallmark USMLE clue is respiratory distress with diffuse crackles in a patient with a cardiac history. Chest X-ray findings include cardiomegaly, Kerley B lines, cephalization, perihilar edema, and pleural effusions. BNP or NT-proBNP helps differentiate cardiac from pulmonary etiologies. The exam prioritizes acute management: oxygen, nitrates, noninvasive ventilation, and IV loop diuretics. If cardiogenic shock is suspected, ultrasound showing reduced EF or severe valvular disease guides vasopressor/inotrope choice. Definitive long-term strategies like ACE inhibitors, beta-blockers, and device therapy appear more on chronic HF questions. COPD exacerbations appear often in Step 2 CK and Step 3 because they test both respiratory physiology and management escalation. Classic findings include wheezing, prolonged expiration, barrel chest, and increased AP diameter. Triggers include viral infections, bacterial infections, and environmental exposures. Initial therapy is standardized: inhaled bronchodilators, systemic corticosteroids, and antibiotics if purulence or increased sputum volume is present. Oxygen must be titrated carefully; excessive oxygen may worsen hypercapnia due to V/Q mismatch. Noninvasive ventilation is a high-yield management step for patients with elevated CO₂ or increased work of breathing. Intubation appears in questions involving altered mental status, severe acidemia, or exhaustion. Pneumonia presents with fever, productive cough, pleuritic pain, and focal crackles. On exams, the presence of fever sharply distinguishes infectious causes from PE or CHF. A patient with lobar consolidations, egophony, and leukocytosis is almost always a pneumonia case unless the vignette suggests aspiration risk or immunocompromise, in which case atypical organisms may appear. Management focuses on obtaining a CXR, assessing severity (eg, CURB-65), and initiating appropriate antibiotics. Severe cases require ICU-level care and broader coverage. On Step 3, sepsis pathways come into play—lactate measurement, repeat fluids, and early antibiotics. MDSteps’ Adaptive QBank includes hundreds of shortness of breath vignettes using this exact algorithmic logic, with automatic flashcard creation for missed questions that you can export directly to Anki. Many learners use the analytics dashboard to identify gaps in pulmonary and cardiovascular reasoning, especially before Step 2 CK. Medically reviewed by: Jordan Reyes, MDUnderstanding the Shortness of Breath Differential Algorithm
Clue PE CHF COPD Pneumonia
Onset Sudden Gradual–acute Gradual Acute with fever Lung Sounds Clear Crackles Wheezes Focal crackles CXR Normal or wedge Cariomegaly, edema Hyperinflation Consolidation Key Test D-dimer/CTA BNP/Echo ABG CXR + culture Step-Wise Algorithm: Stabilize, Separate, and Solve
Pulmonary Embolism: The “Clear Lungs, Sudden Dyspnea” Pattern
Master your USMLE prep with MDSteps.
100+ new students last month.
Acute Decompensated Heart Failure: Fluid Overload & Pulmonary Edema
COPD Exacerbation: Wheezing, Hypercapnia, and Air Trapping
Pneumonia: Infectious Consolidation and Localized Findings
Putting It All Together: A High-Yield Flowchart
1. Assess stability → oxygen, airway, circulation.
2. Clear lungs? → Suspect PE (sudden) or early sepsis.
3. Diffuse crackles? → CHF unless fever → pneumonia.
4. Wheezes + hypercapnia? → COPD exacerbation.
5. Focal consolidation + fever? → Pneumonia.
6. Use targeted testing: CTA for PE, BNP/CXR for CHF, ABG for COPD, CXR/culture for pneumonia.
Rapid-Review Checklist
References
Shortness of Breath Algorithm: PE vs CHF vs COPD vs Pneumonia Explained