This guide provides a complete, high-yield approach to the ED chest pain workup algorithm, optimized for Step 2 CK and Step 3 clinical reasoning. You’ll learn how emergency clinicians rapidly rule out life-threatening causes, order the correct first-line tests, interpret results, and avoid common NBME traps.
Understanding the ED Logic Behind Chest Pain Triage
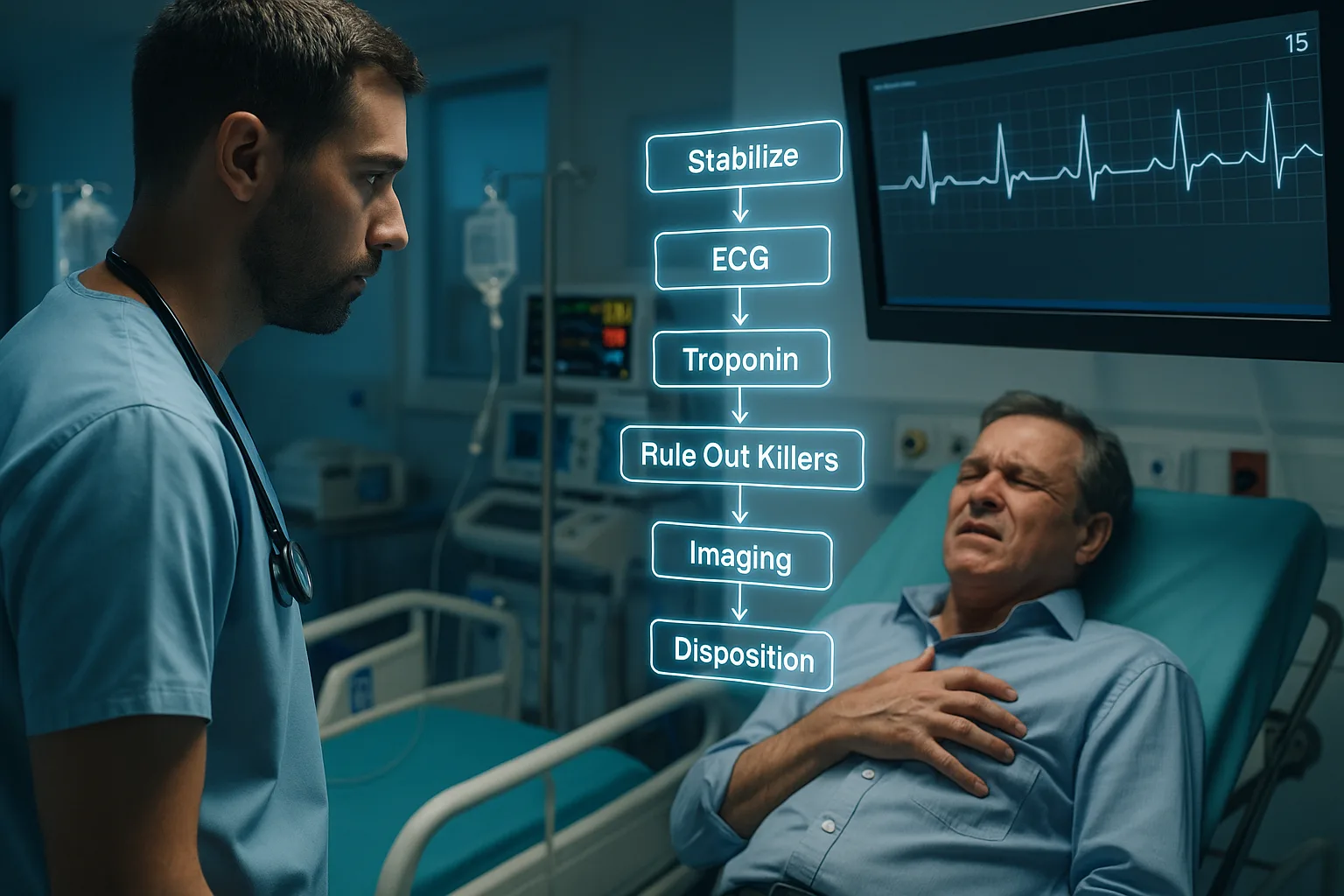
Chest pain is one of the most frequently tested complaints on Step 2 CK and Step 3, precisely because it forces you into rapid prioritization: rule out the killers first, stabilize, risk-stratify, then streamline diagnostic testing. Over both exams, the NBME heavily rewards students who think like ED clinicians—recognizing red flags, interpreting initial data points correctly, and knowing when a finding does not change management.
The ED evaluation follows a strict hierarchy: identify immediate threats (ACS, PE, dissection, tension pneumothorax, tamponade, esophageal rupture), determine stability, acquire essential diagnostics early, and apply validated clinical tools only when safe. Step questions often hinge on knowing when to rely on these tools (e.g., HEART score, Wells, PERC) versus when to bypass them entirely due to instability or exam “danger cues.”
Several distractors appear repeatedly: ordering a stress test during active pain, waiting for troponin trends when ST-elevation is present, or deferring aspirin until after imaging. Your goal in every vignette is to recognize which action changes outcomes immediately—and to act on it. Likewise, many cases use borderline findings such as atypical radiation, mild tachycardia, or nonclassic risk factors to make you reconsider premature closure.
The algorithm below will anchor your thinking for every chest pain presentation. Applying this sequence consistently enhances your accuracy in both emergency medicine vignettes and outpatient follow-up scenarios, since the ED pathway determines subsequent management.
Step 1: Primary Assessment & Stabilization
The first rule of the ED chest pain workup algorithm: treat physiology before diagnostics. Step 2 CK and Step 3 repeatedly test your ability to identify instability early. If the vignette uses phrases like “diaphoretic,” “ashen,” “obtunded,” “severe respiratory distress,” “SBP < 90,” or “gasping,” you must stabilize before considering any formal testing.
- Airway: If altered, vomiting, or obtunded → immediate airway protection.
- Breathing: Oxygen if hypoxic; tension features (tracheal deviation, unilateral absent breath sounds) → needle decompression before imaging.
- Circulation: If hypotensive with JVD → consider tamponade; if hypotensive without JVD → possible massive hemorrhage or cardiogenic shock.
NBME trick: a patient with chest pain and severe dyspnea who is “rapidly deteriorating” should receive stabilization before ECG or CXR—even if ACS is suspected. Management steps always follow the pattern taught by ACLS.
Once stabilized, immediate tests in every chest pain vignette include:
- ECG within 10 minutes
- High-sensitivity troponin
- IV access + vitals
- Portable CXR if respiratory component exists
An early aspirin is universally correct unless contraindicated. Step 3 frequently tests whether you recognize that aspirin comes before troponin results or cardiology consultation. Many examinees mistakenly delay this intervention—resulting in missed points.
Step 2: Rapid ACS Identification & First-Line Actions
Acute coronary syndrome accounts for the highest-stakes decisions during chest pain evaluation. The NBME expects you to rapidly differentiate STEMI from NSTEMI and unstable angina based on ECG clues and symptom evolution.
STEMI: New ST-elevation in ≥2 contiguous leads or posterior ST depression + tall R waves. Immediate reperfusion is the only acceptable next step. The exam may allow fibrinolysis if PCI is unavailable within guideline windows.
NSTEMI: Troponin elevation without ST elevation. Management includes anticoagulation, dual antiplatelet therapy, and risk-guided invasive strategy. Watch for “refractory angina” or “hemodynamic instability”—both mandate urgent catheterization.
Unstable angina: Symptoms consistent with ACS but normal troponins. Treat similarly to NSTEMI until proven otherwise.
| Finding |
STEMI |
NSTEMI |
Unstable Angina |
| ECG |
ST elevation |
ST depression or T-wave inversion |
Normal or minimal changes |
| Troponins |
Elevated |
Elevated |
Normal |
| Immediate Priority |
Reperfuse |
Antithrombotics + risk stratify |
Monitor + repeat testing |
MDSteps’ Adaptive QBank helps reinforce ACS decision-making by surfacing variants of these scenarios, including posterior MI recognition, left main equivalents, and high-risk NSTEMI presentations. Because the QBank adjusts difficulty based on your misses, you repeatedly practice the exact reasoning required to master the ED chest pain workup algorithm.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
Step 3: Identifying Non-ACS Life Threats
After ACS is evaluated, your next priority is excluding the remaining life-threatening causes. The NBME uses structured cues to signal each condition.
Aortic Dissection
- Sudden tearing chest or back pain
- Pulse or BP differential
- Neurologic deficits or acute limb ischemia
First-line test: CT angiography (if stable).
If unstable → bedside TEE is preferred.
Pulmonary Embolism
- Pleuritic pain + dyspnea + tachycardia
- Hemoptysis or recent immobilization
- Clear CXR with hypoxia
Do not apply PERC or Wells if unstable. Straight to CT pulmonary angiography or empiric anticoagulation if shock persists.
Tension Pneumothorax
Clinical diagnosis only. Needle decompression precedes imaging.
Cardiac Tamponade
Beck triad: hypotension, JVD, muffled heart sounds.
First-line test: bedside echo.
Treatment: emergent pericardiocentesis.
Esophageal Rupture
Severe chest pain after vomiting, with subcutaneous emphysema.
First-line test: CT chest with contrast or fluoroscopic esophagram.
Step 4: Imaging Logic on Step 2 CK & Step 3
The exams test your ability to choose the correct imaging pathway based on stability and suspicion level. Memorizing this table saves enormous time:
| Suspected Condition |
Stable |
Unstable |
| PE |
CTPA |
Bedside echo & empiric anticoagulation |
| Aortic Dissection |
CTA chest |
TEE |
| Tamponade |
Echo |
Immediate pericardiocentesis |
| Pneumothorax |
CXR |
Needle decompression |
Step 3 questions commonly require you to choose management before confirmatory imaging if the condition is clinically obvious. This tests whether you prioritize stabilization over diagnostics.
Step 5: Cardiac Biomarkers & Troponin Interpretation
Troponin interpretation is a subtler challenge on both exams. You must differentiate acute MI from chronic elevation and understand the timing of release and clearance.
- Initial troponin may be normal in the first 3 hours of symptoms.
- A rising pattern is more diagnostic than a single abnormal value.
- Chronic elevations (CKD, HF) require serial testing.
NBME trick: If a patient has classic ischemic symptoms + ischemic ECG changes, treat as ACS even before troponins return.
MDSteps’ automatic flashcard generator (exportable to Anki) reinforces these patterns by turning your troponin-related QBank errors into spaced repetition cards—a powerful way to internalize the kinetics and avoid mistakes on test day.
Step 6: Risk Stratification Tools—When to Use & When Not To
The HEART score, Wells criteria, Geneva score, and PERC rule all appear in Step 2 CK/3 vignettes, but the exams emphasize knowing when these tools are appropriate.
- Never apply decision tools in unstable patients.
- PERC is only valid in low-risk patients already deemed low-risk by clinician gestalt.
- HEART is used after initial ACS rule-out, not before ECG or troponin.
NBME distractor: offering a risk score when the patient is in clear distress or when symptoms strongly suggest a dangerous diagnosis. Always bypass scoring tools in these situations.
Rapid-Review Checklist: ED Chest Pain Workup Algorithm
- Stabilize first: airway, breathing, circulation.
- Immediate tests: ECG, troponin, CXR, IV access.
- Give aspirin early unless contraindicated.
- STEMI → immediate reperfusion.
- Unstable patient with chest pain → skip decision rules.
- Aortic dissection: CTA if stable, TEE if unstable.
- PE: CTPA if stable, bedside echo + anticoagulate if unstable.
- Pneumothorax with tension → needle before imaging.
- Tamponade → echo; if shock, pericardiocentesis without delay.
- Never order a stress test during active chest pain.
Mastering this algorithm dramatically improves accuracy across Step 2 CK and Step 3 emergency medicine blocks. For full-length practice, consider MDSteps’ Adaptive QBank and exam analytics dashboard, which present chest pain cases in escalating complexity and help you monitor readiness with objective performance metrics.
References
Medically reviewed by: Jordan Hale, MD, FACEP
100+ new students last month.