Post‑operative fever is a classic topic on Step 2 CK, and the “Wind, Water, Wound, Walk, Wonder Drugs” mnemonic remains the backbone of test‑day reasoning. Within the first 100 words, it’s essential to emphasize that the diagnostic approach to early vs late fever follows a timeline‑driven algorithm rather than reflexive antibiotic use. For the exam, the highest‑yield skill is separating benign post‑surgical inflammatory responses from red‑flag infections requiring immediate workup. Students who excel on these questions pay close attention to the exact postoperative day (POD), the pattern of vitals, and whether the patient has focal symptoms. The timing determines the etiology: “Wind” (atelectasis or pneumonia) dominates POD 1–3, “Water” (UTI) POD 3–5, “Wound” (SSI) POD 5–7, “Walk” (DVT/PE) POD 5+, and “Wonder Drugs” anytime after medication exposure. A key Step 2 CK trap is assuming atelectasis causes fever; while traditional mnemonics include it, modern evidence shows atelectasis alone does not cause significant fever. Exams increasingly test this nuance by presenting early fever but normal imaging. Another common NBME pitfall: giving antibiotics before cultures. Always culture first unless the patient is hemodynamically unstable. MDSteps’ adaptive QBank (9,000+ questions) frequently drills this timeline logic with nuanced distractors that mimic NBME style. This reinforces pattern recognition across repeated exposure, helping learners instantly map POD number → likely cause → appropriate initial test. Early fever in the immediate postoperative window requires rapid assessment of respiratory function, oxygen saturation trends, and risk factors such as smoking, obesity, or prolonged anesthesia. Step 2 CK questions often describe mild fever with decreased breath sounds on POD 1, tempting the student to diagnose pneumonia. However, pneumonia rarely develops this quickly; an infiltrate on CXR is necessary for diagnosis. The exam expects you to distinguish between postoperative atelectasis (common, self‑limited, improved by incentive spirometry) and infectious pneumonia (fever + infiltrate + productive cough). USMLE logic: If fever occurs without respiratory symptoms and imaging is normal, do not treat with antibiotics. Provide pulmonary hygiene and repeat vitals. Conversely, if the vignette mentions purulent secretions, worsening tachycardia, or new oxygen needs, obtain blood cultures, sputum culture, and CXR before starting treatment. This window classically involves urinary tract infections, particularly in patients with prolonged Foley catheterization. Step 2 CK will often include a Foley catheter still in place on POD 3, flank or suprapubic tenderness, or cloudy urine in the collection bag. Always obtain a urinalysis and culture before initiating therapy unless the patient is unstable. A key testing point: removal of the Foley catheter dramatically reduces the risk, and exam writers frequently reward students who recognize unnecessary catheter continuation. Diagnosis is straightforward with pyuria, bacteriuria, and symptoms. Asymptomatic bacteriuria should not be treated except in pregnancy or prior to urologic procedures—another NBME favorite trap. In the postoperative setting, fever + UTI findings → treat with antibiotics targeted to the most common pathogens (E. coli and other Enterobacteriaceae). Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data. By POD 5, wound infections become the leading cause of fever. Superficial SSIs present with erythema, induration, tenderness, and drainage. Deep or organ‑space infections produce systemic toxicity—tachycardia, rigors, persistent leukocytosis. Step 2 CK stresses distinguishing cellulitis (treat with antibiotics alone) from abscess (requires drainage). If fluctuance or purulent material is present, incision and drainage is mandatory. Red flags requiring imaging include crepitus, rapid onset pain out of proportion, or systemic toxicity—raising suspicion for necrotizing soft tissue infection. CT with contrast is appropriate, but unstable patients go directly to surgical exploration. Culture the wound before antibiotics unless septic. Immobility after surgery increases the risk of DVT and PE, typically beginning around POD 5. USMLE vignettes often include unilateral calf pain, swelling, or sudden pleuritic chest pain with tachycardia. The clinical priority is stabilization: assess ABCs, provide oxygen, and evaluate hemodynamics. If PE is suspected in an unstable patient, proceed directly to CT pulmonary angiography or empiric anticoagulation depending on stability and contraindications. Step 2 CK emphasizes that D‑dimer is not useful in post‑op patients because it is nonspecific. Duplex ultrasound is first‑line for suspected DVT. Use clinical findings rather than screening labs to guide diagnosis. Drug fever can occur at any point and is a classic NBME curveball. Culprit medications include beta‑lactams, sulfonamides, heparin, anticonvulsants, and anesthetics. Features include relative bradycardia, rash, eosinophilia, and fever that does not respond to antibiotics. Once suspected, the best next step is discontinuing the offending drug and observing for improvement. Medically reviewed by: John M. Reyes, MDUnderstanding the Post‑Op Fever Framework
POD 1–3: “Wind” — Pulmonary Sources
Finding Atelectasis Pneumonia Timing POD 1–2 POD 2–5 CXR Volume loss Focal/lobar infiltrate O2 need Mild ↑ Moderate–severe ↑ Management Incentive spirometry Antibiotics after cultures POD 3–5: “Water” — Urinary Tract Sources
Master your USMLE prep with MDSteps.
100+ new students last month.
POD 5–7: “Wound” — Surgical Site Infection
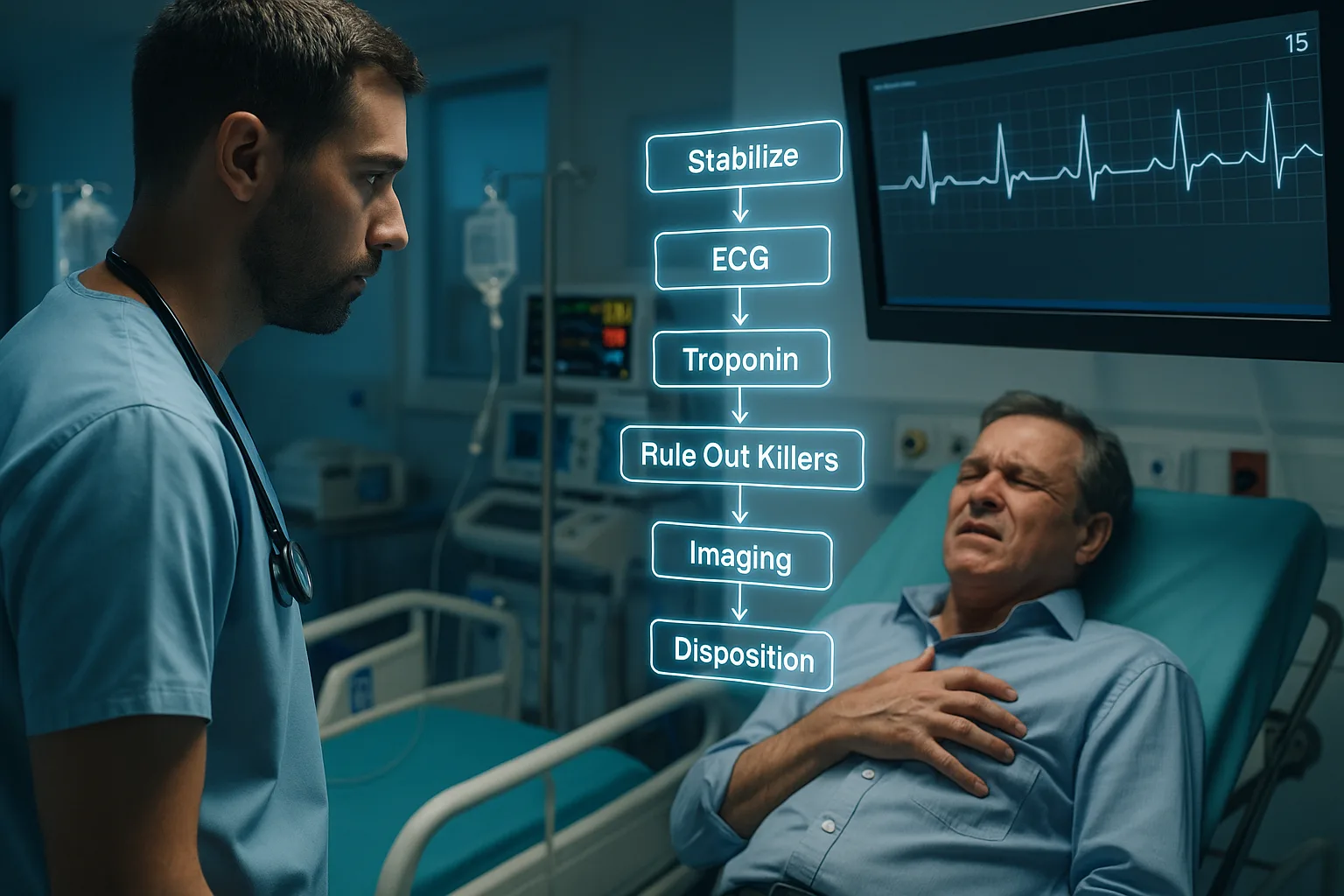
POD 5+: “Walk” — Venous Thromboembolism
“Wonder Drugs”: Medication‑Induced Fever
Diagnostic Algorithm: Putting It All Together
Rapid‑Review Checklist
References
Post‑Op Fever Algorithm: Wind, Water, Wound, Walk, Wonder Drugs for Step 2 CK