The transition from Step 2 CK to Step 3 introduces a fundamental shift in how clinical reasoning is tested. Although both exams rely on patient-centered vignettes, the logic underlying Step 3 questions emphasizes independent decision-making, resource stewardship, and longitudinal patient management. Understanding these contrasts in question logic is central to optimizing preparation, especially as the long-tail query “Step 3 vs Step 2 CK question logic” reflects a growing need to decode what differentiates these two high-stakes examinations.
Step 2 CK focuses heavily on diagnostic accuracy, disease mechanisms, and evidence-based initial management. In contrast, Step 3 often assumes the clinician has already identified the working diagnosis and now must determine the safest next step, adjust therapy over time, or prioritize interventions under constraints such as cost, access, or comorbidities. This introductory section outlines the conceptual framework that will guide the rest of this article: appreciating not only what the exams test, but how they expect you to think. That shift—from identifying the problem to managing a patient over multiple encounters—defines the difference in question logic.
Because Step 3 incorporates Advanced Clinical Medicine (ACM), the reasoning process becomes more operational: what action do you take today, in the correct order, with attention to both safety and long-term outcomes? Step 2 CK rewards recognition; Step 3 rewards synthesis. This article breaks down the unique cognitive demands, common traps, problem-solving patterns, and exam-specific thought processes that distinguish the two exams. Throughout, you’ll find evidence-based learning approaches, schedule optimization tools, and strategic study recommendations.
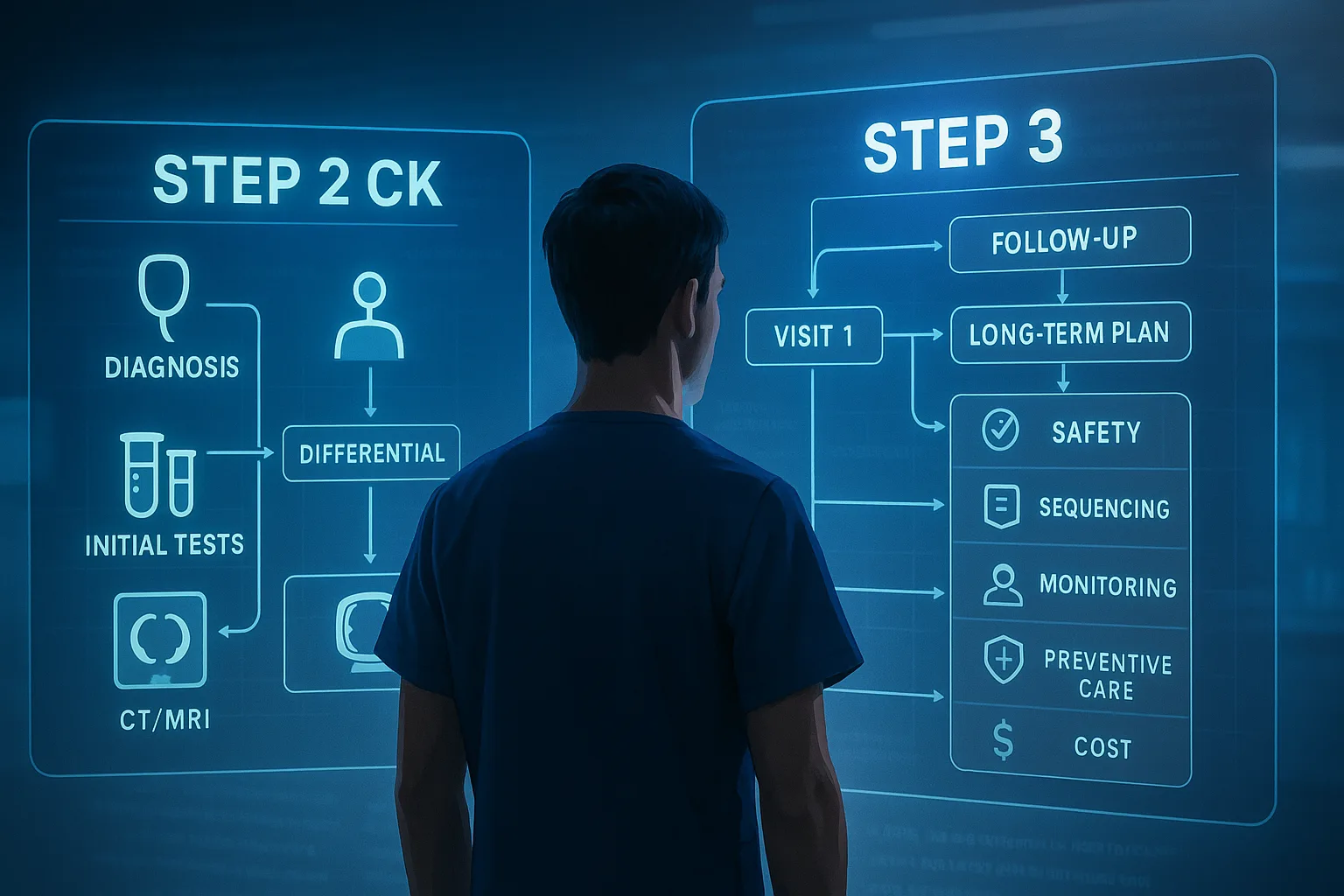
Although both exams use clinical vignettes, the structure and framing of Step 3 items shift the cognitive load in meaningful ways. Step 2 CK typically presents a single encounter, giving clues to identify the disease and choose the best evidence-based diagnostic or treatment option. The question logic is centered on identifying key buzzwords, risk factors, temporal associations, and pathology patterns. Students are expected to diagnose with precision and order tests that confirm or rule out life-threatening conditions.
Step 3 varies the question presentation to reflect a practicing clinician’s broader responsibilities. Many questions simulate continuity of care: a single vignette may unfold over several visits or admissions. Instead of asking, “What is the diagnosis?” Step 3 frequently presents a confirmed diagnosis early and asks what must be done now, in what order, and why. For example, a patient with known heart failure may return with worsening dyspnea after medication nonadherence. The exam will require you to distinguish between urgent and routine interventions, and to weigh the safety implications of diuretic titration versus admission for monitoring.
The question logic also differs in the use of distractors. Step 2 CK distractors usually represent alternative diagnoses or near-correct tests. Step 3 distractors often include interventions that are not wrong but are inappropriate in the moment (too aggressive, unsafe, premature, or economically wasteful). This difference reflects the exam’s emphasis on clinical responsibility. Test writers intentionally embed options that could be reasonable in another context but are inappropriate for the encounter described.
To illustrate these contrasts, consider the following quick comparison:
The heart of the Step 3 vs Step 2 CK question logic divide lies in the shift from diagnostic reasoning to managerial reasoning. Step 2 CK examines your ability to gather clinical clues, apply epidemiologic probability, and rule in or out common conditions. The cognitive sequence resembles: identify → categorize → confirm → treat.
Step 3, however, assumes the diagnosis is known or easily inferable. The cognitive sequence shifts to: stabilize → prioritize → manage → reassess. This requires a deeper understanding of contraindications, drug side effects, monitoring intervals, long-term therapeutic goals, and shared decision-making considerations (e.g., pregnancy safety profiles, renal dosing, or cost barriers).
This change in cognitive load affects how you must study. Step 2 CK prep emphasizes pattern recognition and memorization of high-yield disease associations. Step 3 demands comfort with guideline-driven algorithms and decision trees. For example, while Step 2 CK may ask about diagnosing preeclampsia, Step 3 is more likely to ask about postpartum follow-up, medication continuation, or safety considerations when breastfeeding.
For learners who struggle with the transition, a structured approach is key. Think in terms of “management buckets”: acute interventions, definitive therapy, monitoring, patient education, and preventive strategies. Frameworks like these help predict the logic of Step 3 items. MDSteps’ Adaptive QBank, with its evolving difficulty and analytics dashboard, can assist by highlighting weak management domains and generating targeted flashcards from missed items—useful when refining management-based reasoning.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
Unlike Step 2 CK, Step 3 embeds a population-health lens into its question logic. Students encounter scenarios involving limited access to imaging, insurance restrictions, or community-level interventions. The test writers expect the candidate to navigate these constraints safely while upholding best practices.
This emphasis affects how distractors are constructed. In many Step 3 questions, two or three answer options are medically correct, but only one respects resource stewardship principles. For example, prescribing an expensive new medication without trialing a generic equivalent first may be incorrect not because of clinical harm but because it violates cost-conscious care principles. Step 3 rewards clinicians who understand stepwise escalation and who reserve specialized interventions for appropriate cases.
Another dimension is preventive medicine logic. While Step 2 CK tests screening recommendations as facts, Step 3 tests screening decisions as context-dependent actions. A 55-year-old smoker may need lung cancer screening, but whether that is the most appropriate next step depends on the vignette’s clinical context. This nuanced reasoning is central to Step 3 logic.
Mastering this content requires deliberate practice. Table-based review of screening intervals, risk thresholds, and guideline nuances can be particularly powerful. Equally important is learning to balance individual versus population-level benefit. Because Step 3 cases often integrate multiple guideline elements, familiarity with USPSTF, ADA, and IDSA recommendations is essential.
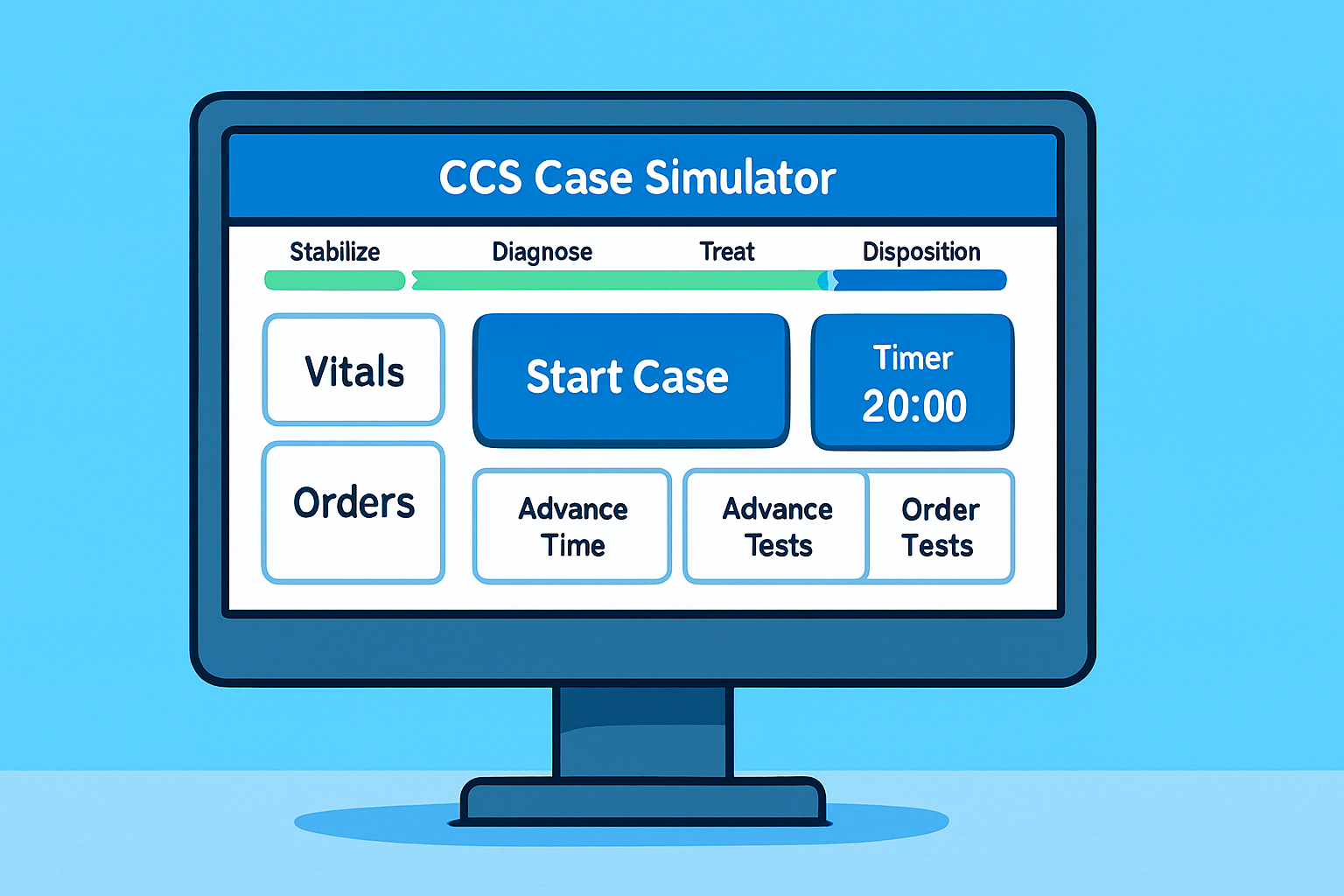
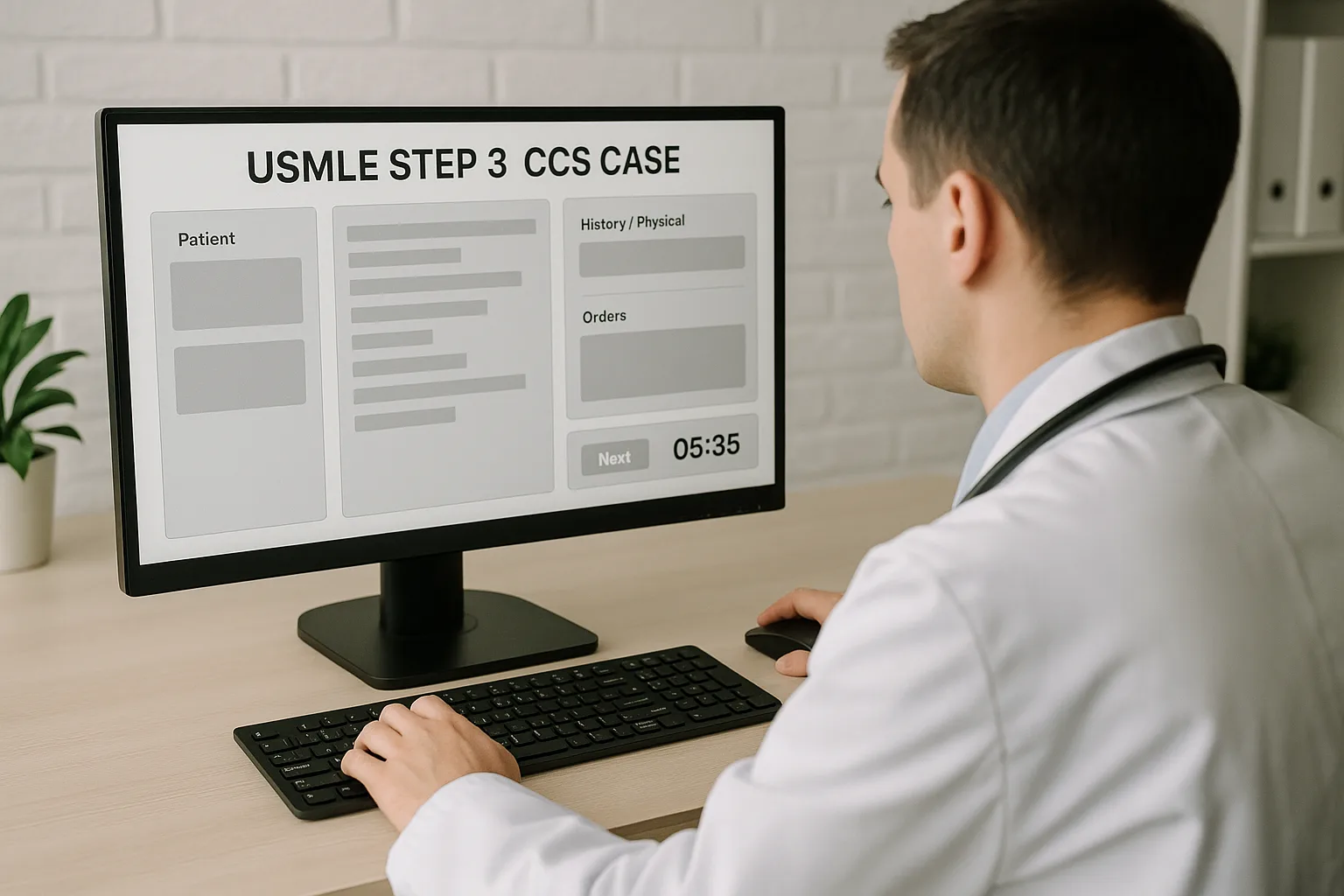
Even though both exams use multiple-choice formats, their pacing influences question logic. Step 2 CK requires efficient interpretation of long vignettes but does not force the multi-step reasoning seen in Step 3’s multiple encounters. Step 3 incorporates fatigue testing: long blocks, multi-day examination structure, and CCS Cases that require real-time decisions. This design element forces examinees to think beyond recall and to rely on internalized clinical models.
Effective test takers develop “mental models” for common conditions. These models integrate red flags, time-sensitive decisions, and long-term goals. For example, a mental model for sepsis includes immediate stabilization, timely antibiotics, fluid resuscitation targets, and monitoring. Step 2 CK may test early recognition; Step 3 tests sequencing and reassessment.
To optimize performance, students benefit from timed question sets and scenario-based practice. MDSteps provides live Vitals CCS Cases for Step 3, allowing realistic simulation of management sequences—highly effective for internalizing question logic. Practice improves not only content mastery but also cognitive endurance.
Recognizing distractor patterns is essential for excelling on both exams. Step 2 CK relies on distractors that mimic similar diseases (Crohn vs UC), competing diagnostic tests (CT vs MRI), or near-correct treatments (azithromycin vs doxycycline). These reward precise knowledge.
Step 3 distractors focus on mis-sequencing. The wrong answer is often a right action at the wrong time. For example, giving high-dose steroids before excluding infection, or ordering MRI before stabilizing a trauma patient. The exam penalizes unsafe practice more than lack of knowledge.
Common Step 3 distractor types include:
Learning these patterns helps decode the exam’s logic. Students should annotate QBank reviews with notes about why distractors fail—this builds a meta-awareness of test writer habits.
A well-structured study plan acknowledges that Step 2 CK and Step 3 demand distinct but related skill sets. For Step 2 CK, foundational science, diagnostic reasoning, and guideline recall dominate. Step 3 requires management fluency and continuity-of-care reasoning.
An effective schedule includes:
Students rotating clinically can leverage downtime effectively using MDSteps’ automatic study plan generator and adaptive flashcards created from QBank misses—especially helpful for reinforcing management sequences required for Step 3.
Medically reviewed by: Priya Nandakumar, MDUnderstanding Step 3 vs Step 2 CK Question Logic
How Question Presentation Drives Reasoning on Each Exam
Feature
Step 2 CK
Step 3
Primary focus
Diagnosis, initial tests, first-line treatment
Management sequencing, long-term care, safety
Common question style
Single encounter vignette
Multi-encounter or follow-up scenario
Distractor type
Alternate diagnoses or incorrect tests
Over- or under-management, unsafe timing, cost-inefficient options
Assumed knowledge
Recognition of pathology
Application of guidelines across evolving contexts
Decision-Making vs Diagnosis: A Shift in Cognitive Load
Master your USMLE prep with MDSteps.
100+ new students last month.
How Step 3 Incorporates Population Health and Resource Stewardship
Timing, Test Flow, and Mental Modeling Differences
Common NBME Traps and Distractor Patterns
Building a Study Plan for Mastering Both Exams
Rapid-Review Checklist: Step 3 vs Step 2 CK Question Logic
References
Step 3 vs Step 2 CK: Key Differences in Question Logic