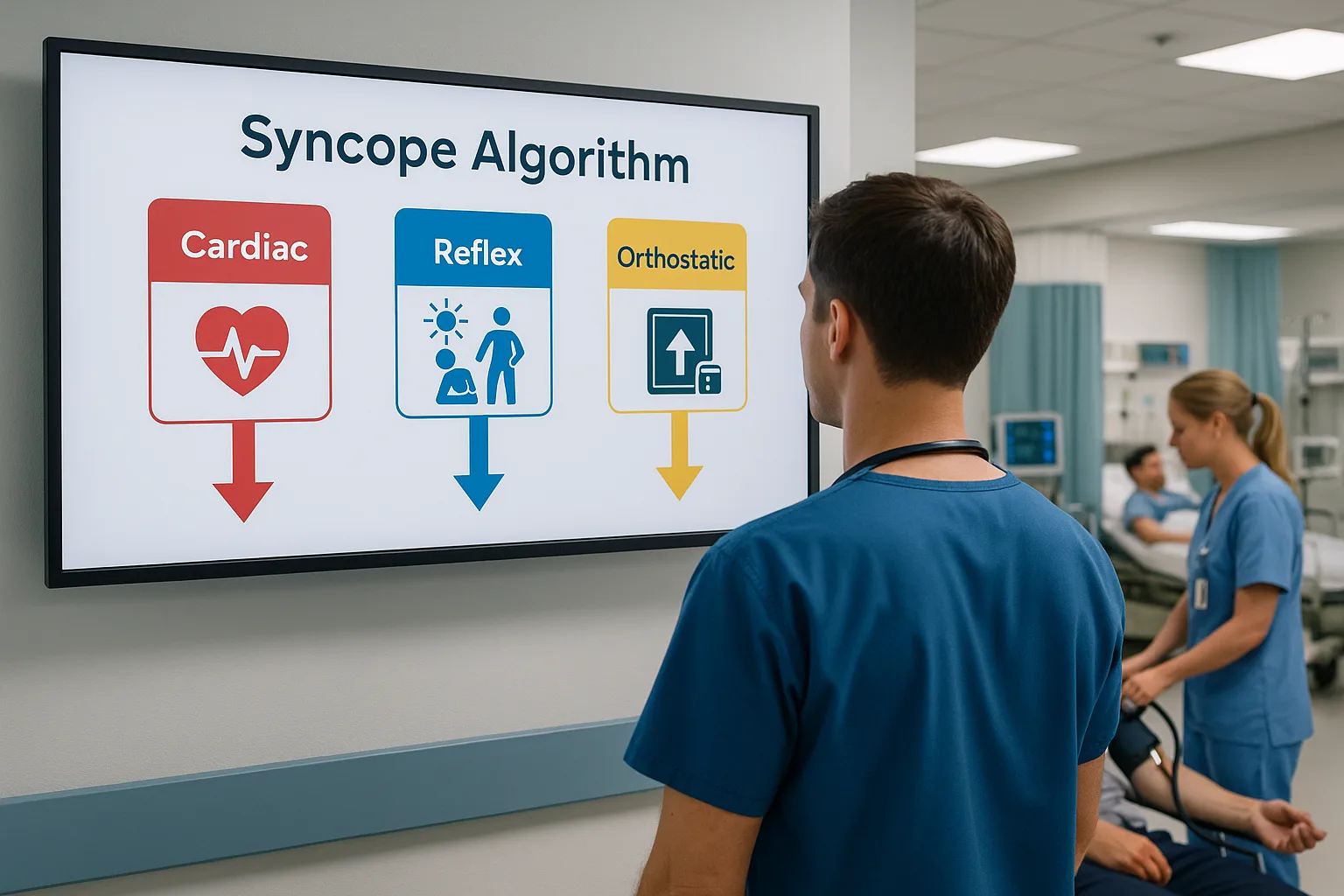
Understanding the Syncope Diagnostic Algorithm for Cardiac, Reflex, and Orthostatic Causes
Syncope remains a high-yield topic for Step 2 CK because it blends cardiovascular physiology, autonomic regulation, and rapid bedside decision-making. The heart of scoring points on these questions is recognizing which mechanism—cardiac, reflex, or orthostatic—best fits the clinical presentation. In this guide, we break down the syncope diagnostic algorithm for cardiac vs reflex vs orthostatic etiologies, emphasizing pattern recognition, red-flag identification, and NBME-style distractors.
Candidates often struggle not because the physiology is difficult, but because the real exam hinges on distinguishing the immediately dangerous cardiac causes from benign reflex (neurally mediated) episodes and iatrogenic or volume-related orthostatic drops. The goal of this algorithm is to simplify that initial branching decision by teaching you to identify high-risk clues within the first ten seconds of reading a vignette. Once this “first branch” becomes automatic, you will notice a major improvement in timing and accuracy.
The Step 2 CK emphasis trends toward:
- Identifying high-risk cardiac etiologies requiring urgent evaluation (arrhythmias, obstructive lesions, ischemia).
- Recognizing classic triggers of reflex syncope (emotional stimuli, prolonged standing, procedural triggers).
- Interpreting orthostatic vitals and medication-induced hypotension correctly.
- Making evidence-based decisions consistent with guideline-driven management.
The MDSteps adaptive QBank frequently tests these clinical patterns using physiology-driven stems and timed ECG spot diagnosis. If you want to reinforce each branch of the algorithm, our analytics dashboard helps isolate specific weak domains—for example, distinguishing vasovagal from ventricular tachyarrhythmia presentations. We include similar clinical logic here so you can apply the algorithm immediately.
| Etiology |
Key Trigger |
Exam Clue |
Risk Level |
| Cardiac |
Exertion, supine episodes, palpitations |
Abnormal ECG, structural heart disease |
High |
| Reflex |
Emotional distress, pain, standing |
Prodrome, rapid recovery |
Low |
| Orthostatic |
Position change |
Positive orthostatics, dehydration, medications |
Moderate |
Your job is to internalize the logic behind this table. Once you can consistently identify the initial branch point, Step 2 CK syncope questions become significantly easier. Cardiac etiologies get ruled in or ruled out in the first two sentences of nearly every NBME stem. Reflex syncope is the diagnosis only when “dangerous features” are absent. Orthostatic causes rarely appear without medication clues or volume loss.
Cardiac Syncope: When the Exam Wants You to Act Fast
In the syncope diagnostic algorithm for cardiac vs reflex vs orthostatic etiologies, the cardiac pathway is the only one associated with immediate morbidity and mortality. This makes it the most important branch to recognize rapidly. Cardiac syncope occurs when cerebral perfusion drops abruptly due to arrhythmias, mechanical obstruction, or impaired output. Because these patients can deteriorate quickly, Step 2 CK emphasizes red flags that strongly predict a cardiac mechanism.
High-yield cardiac clues include:
- Syncope during exertion (think aortic stenosis, HOCM, arrhythmias).
- No prodrome—loss of consciousness is sudden and unexpected.
- Syncope while supine—reflex causes rarely happen lying down.
- Palpitations preceding syncope—suggest tachyarrhythmia.
- Abnormal ECG—long QT, Brugada, WPW, heart block, ischemia.
- Family history of sudden cardiac death.
The exam frequently uses the “exertional athlete collapse” scenario. If a young athlete passes out during physical activity, you should instantly think of HOCM or arrhythmogenic disorders unless proven otherwise. Another classic pattern is the elderly patient collapsing while walking uphill or climbing stairs, hinting at severe aortic stenosis. Both require echocardiography as the next diagnostic step.
Arrhythmias constitute the most common cardiac etiology tested. Ventricular tachycardia produces syncope due to sudden loss of output, while AV block causes prolonged pauses. The key exam move is straightforward: if the ECG is abnormal, the diagnosis is cardiac until proven otherwise.
| ECG Finding |
Likely Cause |
Next Step |
| Long QT |
Torsades risk |
Stop offending drugs, Mg |
| Deltawave |
WPW pathway |
EP study if symptomatic |
| Brugada pattern |
Sodium channelopathy |
ICD evaluation |
| LVH + systolic murmur |
HOCM |
Echocardiogram |
A Step 2 CK pitfall is mislabeling a cardiac episode as vasovagal because the patient “felt nauseated” afterward. Recovery symptoms do not define the mechanism; what matters is the onset. Reflex syncope has a prodrome before loss of consciousness, not afterward. This alone resolves many distractors on exam day.
Reflex (Vasovagal) Syncope: Recognizing Benign Physiologic Responses
Reflex syncope, also known as vasovagal or neurally mediated syncope, is the most common benign cause of transient loss of consciousness. In the syncope diagnostic algorithm for cardiac vs reflex vs orthostatic etiologies, this mechanism is identified by a characteristic prodrome and a clear physiologic trigger. Most Step 2 CK questions will reward you for identifying these hallmark clues.
High-yield reflex triggers:
- Pain, emotional stress, fear (blood draws, needles, childbirth discussion).
- Prolonged standing or heat exposure.
- Post-micturition or defecation syncope.
- Situational triggers such as coughing or swallowing.
The prodrome is what makes this mechanism easy to differentiate. Symptoms typically include:
- Lightheadedness
- Nausea
- Warmth or flushing
- Diaphoresis
- Visual dimming or tunnel vision
Importantly, reflex syncope produces a slow, graceful loss of consciousness—not a sudden collapse. A patient may describe “falling to their knees,” which never happens in arrhythmic syncope. Recovery is rapid but not instantaneous, and the patient often feels fatigued afterward.
Step 2 CK often includes tilt-table testing in questions where the diagnosis is unclear. A positive tilt-table test strongly favors reflex syncope, particularly when upright posture induces vasodilation or bradycardia. However, most cases require no advanced testing—the diagnosis is clinical.
| Feature |
Reflex Syncope |
Cardiac Syncope |
| Prodrome |
Present |
Absent |
| Trigger |
Emotional/painful events |
Exertion, sudden |
| ECG |
Normal |
Often abnormal |
| Risk |
Low |
High |
Because reflex episodes are benign, management focuses on reassurance, hydration, and avoidance of triggers. The exam rarely tests pharmacologic therapy for reflex syncope. Instead, it highlights when not to pursue unnecessary cardiac workup. Distinguishing reflex syncope from orthostatic hypotension completes the diagnostic triad and will appear in several exam vignettes.
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
What you get
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
No Commitments • Free Trial • Cancel Anytime
Create your account
Orthostatic Syncope: Identifying Volume Loss, Autonomic Failure, and Medication Effects
Orthostatic hypotension represents the third essential branch of the syncope diagnostic algorithm for cardiac vs reflex vs orthostatic etiologies, and Step 2 CK frequently tests it through straightforward but clinically realistic vignettes. Orthostatic syncope occurs when an inadequate autonomic response to standing causes a sudden drop in cerebral perfusion. Unlike reflex syncope, which is mediated by inappropriate vasodilation and bradycardia, orthostatic hypotension stems from impaired vascular tone or insufficient intravascular volume. Recognizing the specific patterns can transform these questions from ambiguous to predictable.
Typical triggers include standing from a seated or supine position, early-morning ambulation, postprandial states, or medication-induced vasodilation. Patients frequently report symptoms such as lightheadedness, visual dimming, or “about to black out” immediately after rising. A complete loss of consciousness may occur but is usually brief, and recovery occurs once the patient returns to the horizontal position. Step 2 CK frequently provides orthostatic vital signs to confirm the etiology—defined as a drop in systolic blood pressure by at least 20 mmHg or diastolic by at least 10 mmHg within three minutes of standing (per guidelines).
High-yield contributors include:
- Hypovolemia: dehydration, vomiting, diarrhea, bleeding, diuretics.
- Medication effects: antihypertensives, nitrates, alpha-blockers, antipsychotics.
- Autonomic failure: diabetes mellitus, Parkinson disease, amyloidosis.
- Prolonged bed rest leading to impaired autonomic conditioning.
On Step 2 CK, it is crucial to differentiate orthostatic hypotension from reflex syncope, especially when both involve upright posture. Reflex syncope requires emotional or situational triggers and a reproducible prodrome; orthostatic episodes, however, hinge on the act of rising itself. Likewise, reflex syncope rarely produces significant blood pressure changes captured on orthostatic testing, whereas orthostatic hypotension is visibly documented by measurable hemodynamic shifts.
| Cause |
Distinguishing Clues |
Next Step |
| Hypovolemia |
Dry mucous membranes, tachycardia, history of fluid losses |
IV fluids |
| Medication-induced |
Recent med changes, alpha-blockers, antihypertensives |
Adjust medications |
| Autonomic failure |
Older age, diabetes, neurodegenerative disease |
Compression stockings, midodrine |
Management focuses on identifying the underlying cause. Where the exam tests medication side effects, the correct answer often involves dose reduction, discontinuation, or substitution. In hypovolemic states, isotonic fluids reliably reverse orthostatic symptoms and remain a common next step in NBME-style paths. In chronic autonomic dysfunction, non-pharmacologic interventions such as physical counterpressure maneuvers and compression garments predominate. Pharmacologic therapy with agents such as midodrine or fludrocortisone may appear, but are typically reserved for Step 3.
The Complete Syncope Decision Algorithm: A Step 2 CK Pattern-Recognition Tool
Integrating the full syncope diagnostic algorithm for cardiac vs reflex vs orthostatic etiologies allows you to rapidly classify any Step 2 CK syncope vignette. While the exam may disguise distractors using age, comorbidities, or misleading descriptions of “dizziness,” the underlying diagnostic structure remains consistent. This section condenses the algorithm into a practical, exam-ready framework that will allow you to triage stems in under 10 seconds.
High-Yield Syncope Algorithm (Compact Flowchart)
| 1. Initial Clue? |
Exertional? Supine? Palpitations? Abnormal ECG? → Cardiac |
| 2. Trigger Present? |
Emotional, painful, heat, prolonged standing → Reflex |
| 3. Positional Change? |
Symptoms immediately upon standing → Orthostatic |
| If uncertain: |
Check orthostatics → If normal, evaluate for reflex; if abnormal, treat as orthostatic. |
This algorithm mirrors NBME logic exactly. The exam rewards students who treat the question as a branching decision tree rather than a list of symptoms to memorize. When the stem presents exertional syncope or an abnormal ECG, the path ends immediately—you diagnose cardiac syncope. When the vignette showcases an emotional trigger or prolonged standing with a prodrome, reflex syncope becomes the likely answer. When the episode is clearly positional or worsens with dehydration or medication changes, orthostatic hypotension rises to the top of the differential.
MDSteps' adaptive QBank uses this same algorithmic structure in syncope cases, presenting you with variable difficulty ECGs, subtle trigger-word stems, and advanced analytics that reveal whether you misclassify reflex episodes as orthostatic or overlook cardiac red flags. If you want to internalize this decision-making style, the performance dashboard highlights patterns of error and automatically builds flashcard decks from your misses, which can be exported directly into Anki.
NBME-Style Traps and How to Recognize Them in Syncope Questions
Step 2 CK includes several predictable traps within syncope vignettes, and mastering them can significantly improve your diagnostic precision. These traps typically revolve around misleading prodromes, irrelevant comorbidities, or partially redacted histories that hide key clues. Understanding these patterns allows you to differentiate between misleading details and high-yield diagnostic signals.
One common trap involves post-event symptoms mistaken for prodrome. For example, a patient may report nausea or sweating after regaining consciousness. Students sometimes incorrectly attribute these to a reflex mechanism, but reflex syncope requires the prodrome immediately preceding the event. Post-event symptoms offer no diagnostic clarity and should never override red-flag features or ECG abnormalities.
Another trap features elderly patients with multiple comorbidities. The exam may include diabetes, hypertension, coronary artery disease, or autonomic neuropathy to suggest competing diagnoses. However, Step 2 CK always anchors the correct answer to the dominant clinical pattern. A diabetic patient with syncope after standing likely has orthostatic hypotension; the same patient collapsing mid-exertion with no warning should immediately raise concern for a cardiac mechanism regardless of comorbidities.
The “ECG is normal so it’s reflex syncope” trap also appears frequently. A normal resting ECG excludes some but not all arrhythmias. The key is the absence or presence of triggers. If no emotional trigger exists and the event occurs unpredictably, reflex syncope becomes unlikely. Conversely, if orthostatic vitals are normal and the ECG is unremarkable, a reflex mechanism becomes more plausible—provided the clinical setting aligns.
| Trap |
Why It Works |
Correct Interpretation |
| Post-event nausea |
Mimics reflex symptoms |
Not diagnostic—look at pre-event clues |
| Chronic comorbidities |
Distract from red flags |
Focus on trigger and onset pattern |
| Normal ECG |
False reassurance |
Still consider cardiac if onset is sudden |
Ultimately, NBME syncope questions reward consistency: prodrome-heavy → reflex; position-dependent → orthostatic; exertional or sudden → cardiac. Once you internalize this logic, the distractors lose their power.
Applying the Algorithm in Complex Step 2 CK Vignettes
Real exam questions often layer multiple conditions, medications, or environmental factors. This section demonstrates how to apply the syncope diagnostic algorithm for cardiac vs reflex vs orthostatic etiologies to more challenging scenarios, including multi-morbid patients and ambiguous histories. The key is identifying the anchor clue—the detail that carries the highest diagnostic weight.
Consider a 72-year-old man with diabetes, on tamsulosin, presenting with syncope while urinating. At first glance, the event sounds orthostatic because of his autonomic dysfunction and medication list. But the situational trigger—post-micturition—strongly indicates reflex syncope. The anchor clue overrides comorbidities. Conversely, a patient collapsing suddenly without prodrome during physical exertion remains cardiac until proven otherwise, even if they are on vasodilators or dehydrated.
When ECG abnormalities are present, they almost always trump other details. A patient with a prolonged QT interval, even if dehydrated, should be considered at high risk for ventricular arrhythmias. Similarly, a patient with bifascicular block or new conduction delay should push you toward a cardiac pathway unless the trigger is overwhelmingly convincing for reflex or orthostatic causes.
Another high-yield challenge appears in patients with vague or incomplete histories. If the stem notes “she felt dizzy and then passed out,” the exam expects you to differentiate dizziness from presyncope. Lightheadedness on rising suggests orthostatic hypotension; dizziness unrelated to position but associated with emotional distress implies reflex syncope. Syncope without warning remains cardiac until other mechanisms are convincingly demonstrated.
The most advanced NBME-style stems include multiple plausible distractors. Here the algorithm is especially useful: first rule out cardiac causes by scanning for red flags and ECG clues. If none exist, look for triggers pointing to reflex etiologies. If still unclear, examine positional relationships and orthostatic vitals. Applying this structured approach ensures that you remain consistent, efficient, and clinically accurate under timed conditions.
Rapid-Review Checklist for Syncope on Step 2 CK
Below is a condensed, exam-day ready checklist summarizing the syncope diagnostic algorithm for cardiac vs reflex vs orthostatic causes. Use this during last-minute review or when practicing timed blocks.
- Sudden, no warning? → Cardiac.
- Occurs during exertion? → Cardiac.
- Occurs while supine? → Cardiac.
- Palpitations before syncope? → Arrhythmic cardiac cause.
- Emotional stress, pain, needles? → Reflex.
- Prodrome: nausea, warmth, sweating? → Reflex.
- Standing for long periods? → Reflex or orthostatic—use vitals.
- Immediately after standing? → Orthostatic.
- Positive orthostatics? → Orthostatic.
- Med changes (e.g., tamsulosin, antihypertensives)? → Orthostatic.
- Normal ECG + trigger present? → Reflex.
- Normal ECG + no trigger + positional change? → Orthostatic.
Applying this checklist during practice reinforces pattern recognition and helps you avoid NBME traps by relying on structured logic rather than isolated symptoms.
References
Medically reviewed by: Jonathan Reyes, MD
100+ new students last month.