Why Rate-Limiting Enzymes Matter on Step 1 (and How Stems Signal Them)
Rate-limiting enzymes (RLEs) define bottlenecks in metabolic pathways—the slowest, most regulated steps that determine pathway flux. Step 1 exploits these choke points with clinical context (fed vs fasting, exercise, hypoxia, toxins, medication effects) and biochemical clues (ATP/AMP, NADH/NAD+, citrate, fructose-2,6-bisphosphate). Learning the short list of high-yield RLEs and their regulators lets you predict pathway direction and identify the single enzyme the test-writers want.
What makes an RLE testable? (1) It is highly regulated (allosteric or covalent), often at the crossroads of competing pathways; (2) it integrates hormonal state via second messengers (PKA/PKB/AMPK); (3) it is associated with classic poisons, drug targets, or inherited deficiencies; (4) it shows reproducible physiologic shifts between liver and muscle. These properties create predictable stem “scaffolding.”
Decode stems in three moves: State → Regulator → Direction. First, identify physiologic state (postprandial insulin surge, prolonged fasting, anaerobic exercise, ethanol load). Second, translate state into regulators: insulin/PKB promotes dephosphorylation (glycogen synthase on; hormone-sensitive lipase off), glucagon/epinephrine/PKA promote phosphorylation (glycogen phosphorylase on in liver; pyruvate kinase off in liver), AMPK senses energy stress (AMP up). Third, choose the direction of flux and the one enzyme that fits the stem’s lab or vignette clue.
Common traps and how to avoid them: (a) Confusing PFK-1 (glycolysis RLE) with PFK-2/FBPase-2 (regulates F2,6-BP that in turn governs PFK-1 and FBPase-1). (b) Mixing up CPS-I (mitochondrial, urea cycle; needs N-acetylglutamate) with CPS-II (cytosolic, pyrimidine synthesis; activated by ATP/PRPP, inhibited by UTP). (c) Calling pyruvate dehydrogenase the TCA RLE—isocitrate dehydrogenase is the classic RLE of the cycle; PDH is a key gatekeeper but not the canonical RLE.
Clinically anchored recall: (1) G6PD is the RLE of the HMP shunt—think hemolysis after oxidant stress (sulfa drugs, fava beans, infection). (2) HMG-CoA reductase governs cholesterol synthesis—statins inhibit it. (3) Carnitine acyltransferase I (CPT-I) controls β-oxidation entry—malonyl-CoA blocks it in the fed state. (4) ALA synthase starts heme synthesis—needs B6; lead poisoning inhibits downstream ALAD/ferrochelatase, producing anemia with basophilic stippling.
Exam tactic: When faced with a long stem, jump to the final line and the labs/vitals first. Ask: “Is ATP plentiful or scarce? Is insulin high or low? Are we in liver or muscle?” Then return to the pathway schematic in your head. The RLE answer will often be the enzyme that best integrates those signals, not just any enzyme in the pathway.
Glycolysis ↔ Gluconeogenesis: PFK-1, FBPase-1, Pyruvate Kinase, and F2,6-BP Logic
Core RLEs: PFK-1 (glycolysis) and fructose-1,6-bisphosphatase (FBPase-1; gluconeogenesis). PFK-1 is activated by AMP and fructose-2,6-bisphosphate (F2,6-BP) and inhibited by ATP and citrate. FBPase-1 is inhibited by AMP and F2,6-BP. The liver’s bifunctional enzyme PFK-2/FBPase-2 sets the F2,6-BP level; insulin (via phosphatase) favors the PFK-2 activity → ↑F2,6-BP → drives glycolysis; glucagon/epinephrine (via PKA) favors FBPase-2 → ↓F2,6-BP → favors gluconeogenesis.
Pyruvate kinase (PK) is not the RLE of glycolysis but is heavily tested because liver PK is inhibited by phosphorylation (glucagon/PKA) and by alanine, while activated by fructose-1,6-BP (feed-forward). During fasting, the liver spares pyruvate for gluconeogenesis by turning PK off; in exercise, muscle PK is on to feed ATP production.
| State | Hormones/2nd messenger | F2,6-BP | PFK-1 Flux | FBPase-1 Flux | Net Hepatic Output |
|---|---|---|---|---|---|
| Fed (postprandial) | Insulin ↑, PKB/PP1 (dephos) | ↑ | ↑ (glycolysis) | ↓ (off) | Glucose uptake/storage |
| Fasting (overnight) | Glucagon ↑, PKA (phos) | ↓ | ↓ | ↑ (gluconeogenesis) | Glucose export |
| Exercise (muscle) | AMP ↑, Ca2+ ↑ | N/A (muscle) | ↑ | ↓ | ATP production in muscle |
| Ethanol load | NADH ↑ | ↓ (indirect) | ↓ (OAA → malate) | ↑ (relative) | Hypoglycemia risk |
Vignette patterns: (1) Sepsis or vigorous exercise: AMP up, pH down → PFK-1 on; lactate may rise. (2) Prolonged fasting: low insulin, high glucagon → F2,6-BP down → gluconeogenesis dominates; think FBPase-1 activity. (3) Ethanol-induced hypoglycemia: high NADH drives oxaloacetate to malate, impairing gluconeogenesis; the test often asks why PFK-1 is low (substrate/precursor shunting) or which step in gluconeogenesis is impaired.
Exam tip: If the question mentions the bifunctional enzyme being phosphorylated, pick effects consistent with FBPase-2 activity (low F2,6-BP → gluconeogenesis). If it mentions alanine infusion or fasting glucagon, expect liver pyruvate kinase to be off. If the stem says “AMP is high,” default to glycolysis unless there is overwhelming counter-evidence.
PDH, TCA Control, and Ox-Phos Context: From Thiamine to Cyanide
Canonical RLE: Isocitrate dehydrogenase (IDH) is the classic rate-limiting enzyme of the TCA cycle, activated by ADP and Ca2+ and inhibited by ATP and NADH. A frequently co-tested control point is α-ketoglutarate dehydrogenase (also inhibited by ATP/NADH, requires thiamine, lipoate, FAD, NAD+, CoA), but remember: Step 1 expects you to name IDH as the TCA RLE.
PDH is the gatekeeper. Pyruvate dehydrogenase is not the TCA RLE, yet it frequently determines carbon entry. PDH requires the “TLC For Nancy” cofactors (Thiamine, Lipoic acid, CoA, FAD, NAD+). It is inhibited by acetyl-CoA/NADH and activated by dephosphorylation (insulin in adipose). PDH deficiency (often X-linked) presents with lactic acidosis and neurologic deficits; ketogenic diet (lysine/leucine) helps by bypassing PDH.
Ethanol and redox traps: An increased NADH/NAD+ ratio shunts oxaloacetate to malate, limiting gluconeogenesis and pushing pyruvate toward lactate (lactic acidosis). In TCA, high NADH slows IDH—watch for questions where “excess ethanol” or “hypoxia” depresses cycle flux via redox imbalance.
Poison logic you must know: Arsenic inhibits lipoic acid (PDH and α-KG dehydrogenase) → neurologic signs, vomiting, garlic breath. Cyanide/CO disable complex IV in the electron transport chain (hypoxia with normal PaO2, lactic acidosis). Oligomycin blocks ATP synthase; 2,4-DNP uncouples, increasing O2 consumption yet lowering ATP. Step 1 loves to distinguish inhibition (↓O2 use, ↓ATP) from uncoupling (↑O2 use, ↓ATP, heat).
Calcium signaling and exercise: In muscle, Ca2+ released with contraction activates PDH phosphatase and IDH, matching ATP supply to demand. Stems mentioning “skeletal muscle during intense activity” often imply increased TCA flux via Ca2+ and ADP.
Exam tip: If the stem emphasizes malnutrition, hyperemesis, or alcoholism, think thiamine deficiency. Before giving glucose, administer thiamine to avoid precipitating Wernicke encephalopathy; mechanistically, you’re rescuing PDH and α-KG dehydrogenase cofactor needs. If the question ties “almond odor on breath” to lactic acidosis and bright red venous blood, think cyanide—ETC blockade forces glycolysis and lactate production; TCA (and IDH) stall secondarily.
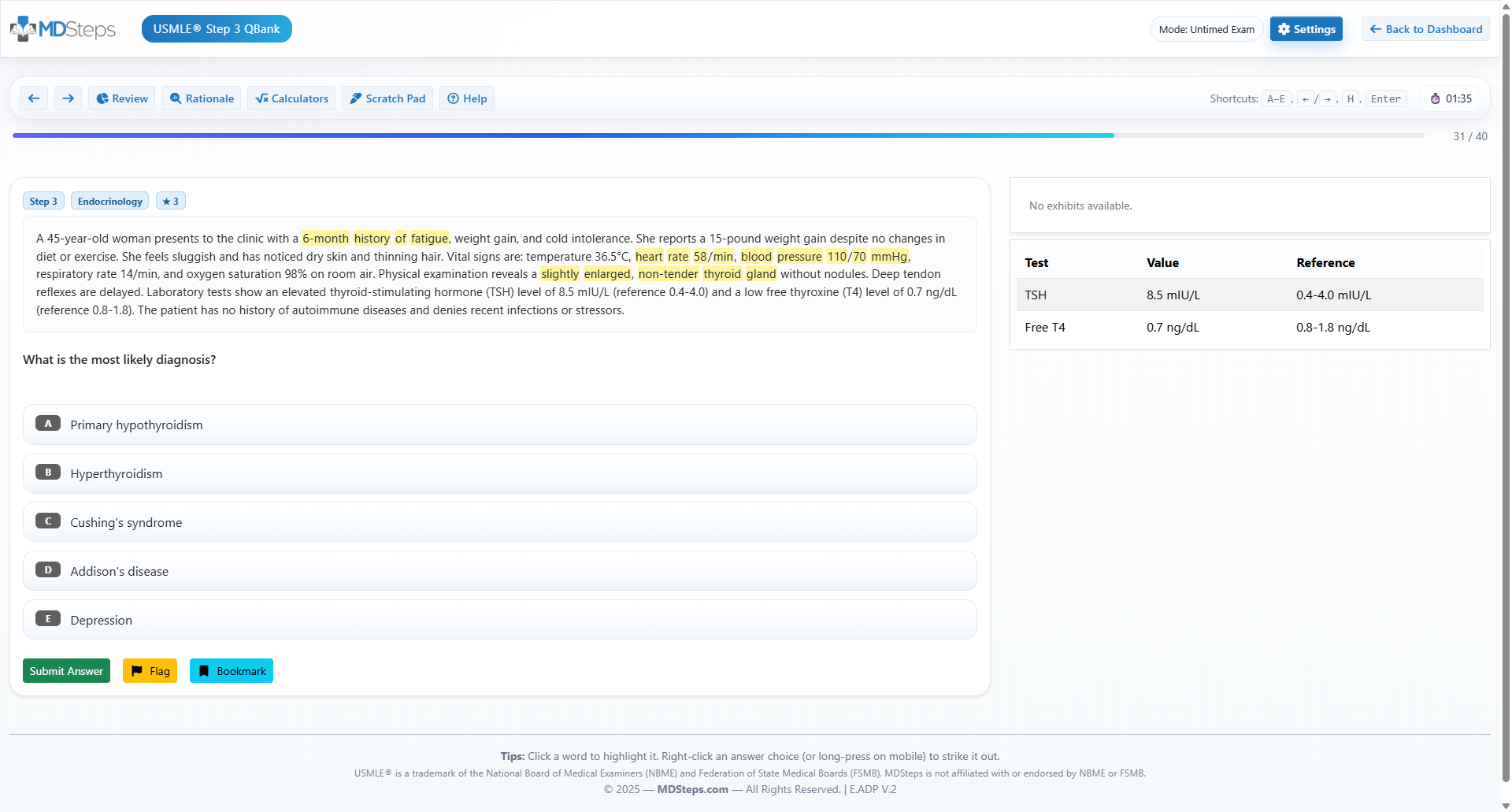
Master your USMLE prep with MDSteps.
Practice exactly how you’ll be tested—adaptive QBank, live CCS, and clarity from your data.
- Adaptive QBank with rationales that teach
- CCS cases with live vitals & scoring
- Progress dashboard with readiness signals
Glycogen Metabolism: Glycogen Synthase & Glycogen Phosphorylase in Liver vs Muscle
Canonical RLEs: Glycogen synthase (glycogenesis) and glycogen phosphorylase (glycogenolysis). The switch tracks hormonal state and tissue. In the liver, glucagon/epinephrine → PKA → phosphorylase kinase activation → glycogen phosphorylase ON (and glycogen synthase OFF). In the muscle, epinephrine and Ca2+ (from contraction) activate phosphorylase kinase; no glucagon receptors here. Insulin promotes dephosphorylation via protein phosphatase 1, turning glycogen synthase ON and glycogen phosphorylase OFF.
Allosteric layers: AMP activates muscle glycogen phosphorylase (low energy state), while ATP and glucose-6-phosphate inhibit it. Liver glycogen phosphorylase is directly inhibited by free glucose, allowing tight regulation of hepatic glucose output when plasma glucose rises—an elegant exam hook.
Clinical anchors: McArdle disease (myophosphorylase deficiency) presents with exercise intolerance, muscle cramps, myoglobinuria, and a “second wind” from increased blood flow; CK is high. Von Gierke (GSD I) is glucose-6-phosphatase deficiency—severe fasting hypoglycemia, lactic acidosis, hyperuricemia, hyperlipidemia. While G6Pase is not the RLE, Step 1 will expect you to predict pathway consequences (glycogen accumulation, impaired gluconeogenesis/glycogenolysis terminal step). Cori (GSD III) (debranching enzyme) features limit dextrins; Pompe (GSD II) (acid α-glucosidase) is lysosomal and classically causes cardiomegaly and hypotonia.
Exam patterns: (1) “Hepatomegaly + fasting hypoglycemia + lactic acidosis” → think GSD I (G6Pase). (2) “Exercise intolerance + myoglobinuria after sprint” → GSD V (myophosphorylase). (3) “Epinephrine/glucagon analog” → favors phosphorylase activation in liver, PKA cascade. (4) “Free glucose infusion” → inhibits liver glycogen phosphorylase (unique liver allostery).
Exam tip: When a stem mentions “phosphorylation state” without naming the enzyme, translate it into the functional pair: phosphorylated form turns glycogen phosphorylase ON and glycogen synthase OFF; dephosphorylation flips the switch. If the vignette lives in muscle, ignore glucagon; rely on epinephrine/Ca2+/AMP. If it lives in liver, integrate glucagon, epinephrine (β and α1), and plasma glucose feedback.
Lipid Pathways: ACC, CPT-I, HMG-CoA Synthase, and HMG-CoA Reductase
Fatty acid synthesis (cytosol): RLE is acetyl-CoA carboxylase (ACC), which converts acetyl-CoA to malonyl-CoA (biotin-dependent). ACC is activated by citrate and insulin (dephosphorylation) and inhibited by glucagon/epinephrine (PKA phosphorylation) and palmitoyl-CoA (product). Malonyl-CoA itself inhibits CPT-I, preventing futile cycling with β-oxidation in the fed state.
β-oxidation (mitochondrial): RLE is carnitine palmitoyltransferase I (CPT-I), which transports long-chain fatty acyl-CoA into mitochondria. In the fasted state, malonyl-CoA levels fall, lifting CPT-I inhibition and permitting fatty acid entry and oxidation. Carnitine deficiency (or CPT-II deficiency) limits β-oxidation → hypoketotic hypoglycemia, muscle weakness, elevated CK, especially with fasting or illness.
Ketogenesis (liver mitochondria): RLE is HMG-CoA synthase. During prolonged fasting or uncontrolled diabetes, hepatic β-oxidation supplies acetyl-CoA, driving ketone production (acetoacetate and β-hydroxybutyrate). Key clinical cue: “fruity breath,” high anion gap metabolic acidosis, and ketonemia—do not confuse this with lactic acidosis from hypoxia/poisoning.
Cholesterol synthesis (cytosol/ER): RLE is HMG-CoA reductase, converting HMG-CoA to mevalonate. It is upregulated by SREBP when intracellular cholesterol is low and inhibited by cholesterol and by statins (competitive inhibitors) which reduce LDL-C and cardiovascular events. Step 1 emphasizes mechanism: decreased hepatic cholesterol increases LDL receptor expression, clearing LDL from plasma.
Vignette patterns: (1) “Well-fed state after carbohydrate-rich meal” → citrate shuttling ↑, ACC active, malonyl-CoA ↑, CPT-I inhibited → FA synthesis on, β-oxidation off. (2) “Prolonged fast/illness in infant with hypoketotic hypoglycemia” → suspect fatty acid oxidation defect (e.g., medium-chain acyl-CoA dehydrogenase deficiency) or carnitine shuttle problem. (3) “New statin with myalgias and elevated CK” → think statin-associated myopathy; mechanism is still HMG-CoA reductase inhibition.
Exam tip: Use malonyl-CoA as your mental toggle. High malonyl-CoA (fed) blocks CPT-I → β-oxidation off. Low malonyl-CoA (fasting) frees CPT-I → β-oxidation on. When the stem mentions citrate, think ACC activation and FA synthesis. When it mentions “competitive inhibitor lowering LDL,” you should be at HMG-CoA reductase in one step.
HMP Shunt, Nucleotides, Urea, and Heme: G6PD, CPS-I vs CPS-II, PRPP Amidotransferase, ALA Synthase
HMP shunt (pentose phosphate pathway): RLE is glucose-6-phosphate dehydrogenase (G6PD). Outputs: NADPH (antioxidant defense, steroid/FA synthesis, respiratory burst) and ribose-5-phosphate (nucleotide precursor). G6PD deficiency → episodic hemolysis with oxidant stress (sulfonamides, dapsone, fava beans, infection); smear: Heinz bodies and bite cells.
De novo purine synthesis: RLE is glutamine-PRPP amidotransferase, inhibited by AMP/GMP/IMP (end-product feedback). Drugs: 6-mercaptopurine/azathioprine inhibit de novo purine synthesis; mycophenolate inhibits IMP dehydrogenase (GMP branch). Lesch-Nyhan (HGPRT deficiency) prevents salvage → ↑PRPP, ↑uric acid, self-injury, dystonia.
De novo pyrimidine synthesis: RLE is carbamoyl phosphate synthetase II (CPS-II) (cytosolic; uses glutamine, CO2, ATP), activated by PRPP and ATP, inhibited by UTP. Contrast with CPS-I in the urea cycle (mitochondrial), which is the urea RLE and requires N-acetylglutamate (NAG) as an obligatory activator; deficiency in NAGS or CPS-I → hyperammonemia without orotic acid elevation. OTC deficiency (X-linked) causes hyperammonemia with orotic aciduria due to carbamoyl phosphate spillover to pyrimidine pathway.
Heme synthesis: RLE is ALA synthase (ALAS; mitochondrial; requires B6). Lead poisoning inhibits downstream ALA dehydratase (ALAD) and ferrochelatase → microcytic anemia with basophilic stippling and elevated zinc protoporphyrin. Liver ALAS1 is induced by barbiturates (↑CYP demand), ethanol, and fasting; erythroid ALAS2 is iron-regulated. Acute intermittent porphyria (porphobilinogen deaminase deficiency) presents with neurovisceral attacks and port-wine urine; treat with hemin to downregulate ALAS1.
Exam patterns: (1) “Neonate with lethargy, vomiting, respiratory alkalosis, normal orotic acid” → think CPS-I/NAGS defects. (2) “Teen with photosensitivity, blistering skin lesions, tea-colored urine” → porphyria cutanea tarda (uroporphyrinogen decarboxylase). (3) “Oxidant drug + back pain + dark urine after infection” → G6PD deficiency. Distinguish salvage vs de novo by PRPP use and end-product controls.
Exam tip: Keep a simple location map: CPS-I = mitochondria (urea); CPS-II = cytosol (pyrimidine). G6PD makes NADPH. ALAS needs B6. Mnemonics are fine, but anchor them to clinical triggers to avoid distractors.
Master Table: Rate-Limiting Enzymes, Regulators, and Locations
| Pathway | Rate-Limiting Enzyme | Key Activators | Key Inhibitors | Compartment | Board Clues |
|---|---|---|---|---|---|
| Glycolysis | PFK-1 | AMP, F2,6-BP | ATP, citrate | Cytosol | Exercise, sepsis → AMP ↑ |
| Gluconeogenesis | Fructose-1,6-bisphosphatase | — | AMP, F2,6-BP | Cytosol | Fasting, glucagon, PKA |
| TCA cycle | Isocitrate dehydrogenase | ADP, Ca2+ | ATP, NADH | Mitochondria | Thiamine, redox state |
| Glycogenesis | Glycogen synthase | Insulin, G6P | PKA (phos), epinephrine | Cytosol | Postprandial storage |
| Glycogenolysis | Glycogen phosphorylase | PKA, Ca2+, AMP (muscle) | Insulin, G6P, ATP; glucose (liver) | Cytosol | Exercise vs fasting |
| FA synthesis | Acetyl-CoA carboxylase | Citrate, insulin | Glucagon/epinephrine, palmitoyl-CoA | Cytosol | Malonyl-CoA ↑ |
| β-oxidation | Carnitine acyltransferase I | — | Malonyl-CoA | Mitochondria | Fasting, carnitine defects |
| Ketogenesis | HMG-CoA synthase | — (substrate-driven) | — | Mitochondria (liver) | Prolonged fasting, DKA |
| Cholesterol synthesis | HMG-CoA reductase | SREBP (low cholesterol) | Cholesterol, statins | ER/Cytosol | LDL receptor upregulation |
| HMP shunt | G6PD | NADP+ | NADPH | Cytosol | Oxidant hemolysis |
| Purine synthesis | Glutamine-PRPP amidotransferase | PRPP | AMP, GMP, IMP | Cytosol | 6-MP/azathioprine |
| Pyrimidine synthesis | CPS-II | ATP, PRPP | UTP | Cytosol | Orotic acid metabolism |
| Urea cycle | CPS-I | N-acetylglutamate | — | Mitochondria | Hyperammonemia patterns |
| Heme synthesis | ALA synthase (B6) | — | Heme, glucose | Mitochondria | Lead, porphyrias |
Rapid-Review Checklist & Exam-Day Essentials
30-second checklist (say it out loud):
- PFK-1 on with AMP/F2,6-BP; FBPase-1 off with the same signals.
- IDH is the TCA RLE; redox and ADP/Ca2+ set its pace.
- Glycogen: PKA → phosphorylase ON, synthase OFF (liver ± muscle differences).
- ACC makes malonyl-CoA (fed → FA synthesis); malonyl-CoA blocks CPT-I.
- HMG-CoA reductase is statin target (↓hepatic cholesterol → ↑LDL receptors).
- G6PD runs HMP; oxidant stress hemolysis = Heinz/bite cells.
- CPS-I (urea, mito) needs N-acetylglutamate; CPS-II (pyrimidine, cyto) inhibited by UTP.
- ALA synthase needs B6; lead blocks ALAD/ferrochelatase.
Time-pressure triage algorithm:
- Identify the organ and state: liver fed/fasting vs exercising muscle.
- Map the signal: insulin/PKB (dephos) vs glucagon/PKA (phos) vs AMPK (energy stress).
- Pick the bottleneck: which single enzyme integrates those signals and explains the labs?
Common confusions fixed:
- PDH vs TCA RLE: PDH is a gatekeeper; isocitrate dehydrogenase is the TCA RLE.
- PFK-1 vs PFK-2: PFK-2/FBPase-2 sets F2,6-BP; PFK-1 is the glycolytic RLE.
- CPS-I vs CPS-II: I = urea/mito/NAG; II = pyrimidine/cyto/UTP inhibition.
- β-oxidation block: in fed state, malonyl-CoA (from ACC) inhibits CPT-I.
Lightning practice prompts
- “Barbiturate use + porphyria flare” → which enzyme to downregulate? (ALA synthase with hemin)
- “Fasting + high acetyl-CoA” → gluconeogenesis or glycolysis? (FBPase-1 on; PK off)
- “Statin started, LDL ↓” → mechanism? (HMG-CoA reductase inhibition → ↑LDL receptors)
- “Fava beans hemolysis” → pathway? (HMP shunt; G6PD)
- “Infant hypoketotic hypoglycemia” → suspect? (FAO/carnitine shuttle defect)
Exam-day rules of thumb
- When in doubt, track phosphorylation: PKA turns catabolism on in liver; phosphatases reverse.
- Use malonyl-CoA as the β-oxidation brake memory peg.
- State the compartment (cytosol vs mitochondria) before picking the enzyme.
- “High NADH” = favor lactate formation and TCA slowdown.
- One strong clinical detail usually maps to one RLE—don’t overthink.
Suggested further reading (open-access where possible):
- Rate-limiting step — overview
- Glycolysis regulation (PFK-1, PK); Gluconeogenesis
- TCA cycle regulation; Electron transport chain
- Pentose phosphate pathway (G6PD)
- Urea cycle (CPS-I, NAG)
- Heme biosynthesis (ALA synthase)
- Fatty acid synthesis (ACC); CPT-I
- Cholesterol biosynthesis (HMG-CoA reductase)
Textbook references: First Aid for the USMLE Step 1 (latest ed.); Lippincott’s Illustrated Reviews: Biochemistry; Lehninger Principles of Biochemistry.